This page provides information form health care providers that have cared for Ms. Morales. It includes some discharge summaries from her oncology care in Columbia, MO, some evaluations on her return to her home in La Plata, and documentation from her short stay at the Northeast Regional Medial Center in Kirksville, Missouri.
Case Notes
Physician & PA
Oncology Discharge Summary - Columbia Hospital
Julia Morales is a 65-year-old female who was diagnosed with small cell lung cancer in 2011. She has been treated with several courses of etoposide and cisplatin, along with radiation therapy. She has not gone into a stable remission.
During this admission she was treated with topotecan, a second line therapy, but did not show any improvement.
She was treated with morphine for continuous severe pain.
Physical Examination:
Pulse 100, Respirations 35, Blood Pressure 130/85, SpO2 90%
General: appears weak and cachectic
Head: normocephalic, atraumatic
Ears: normal
Eyes: Perla, EOMs full, fundi benign
Nose: clear
Throat: no injection, exudate or enlarged tonsils
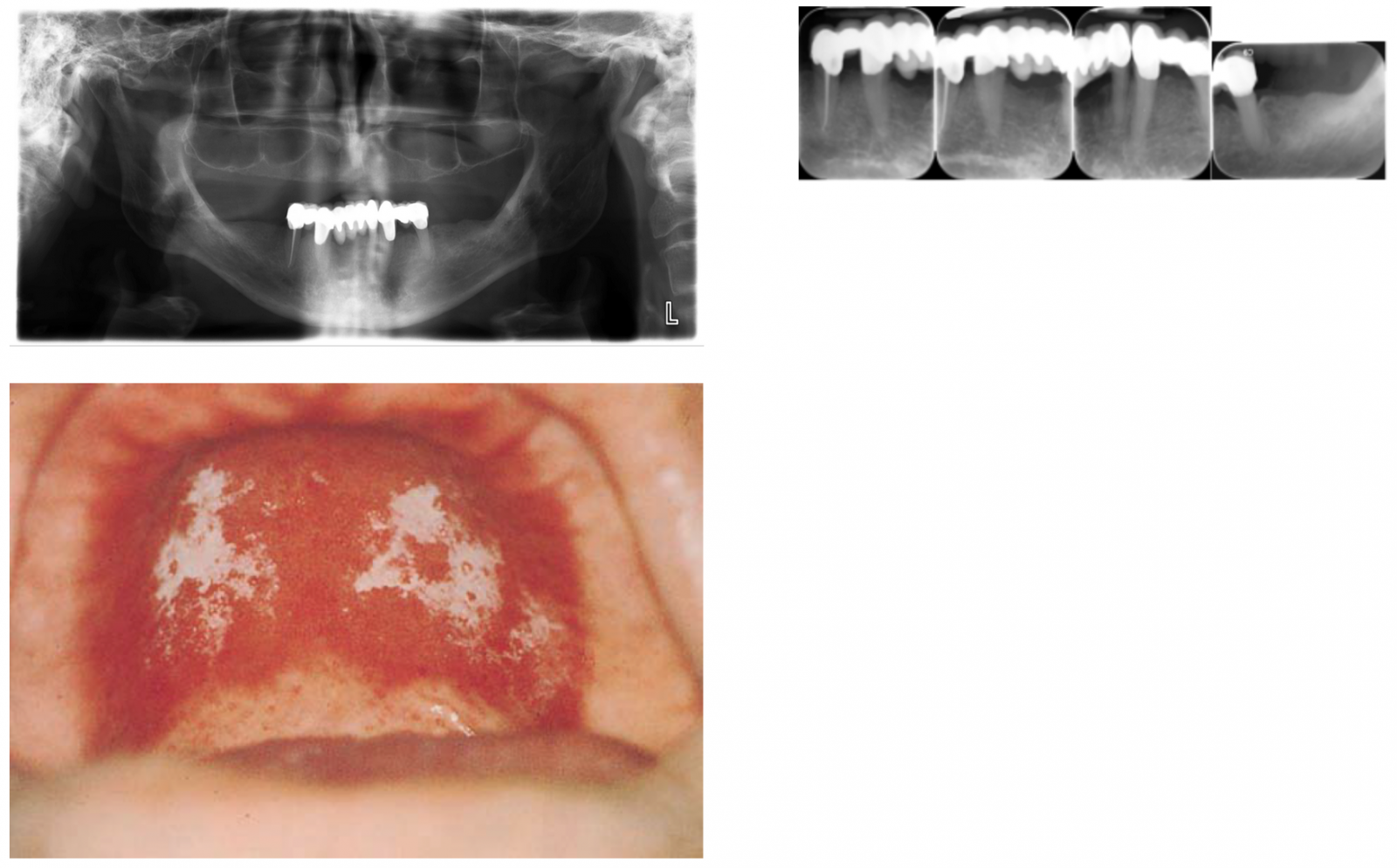
Mouth: Edentulous, patchy white areas on tongue and buccal mucosa
Chest: erythema of anterior chest on right, coarse rhonchi on right upper lobe with decreased air movement, no rales or wheezing
Breasts: no mass or discharge
Heart: regular rhythm, no murmurs
Abdomen: soft, non-tender, no hepatosplenomegaly, bowel sounds present in all quadrants
Genitourinary: No CVA tenderness, normal postmenopausal female genitalia
Extremities: decreased muscle mass and decreased strength in all extremities, decreased tone in all extremities, cranial nerves intact
Neurology: deep tendon reflexes 1+ and symmetric, slow rapid alternating movements, cannot heel-toe walk
Assessment:
- Small cell lung cancer right upper lobe, non-responsive to treatment
- Cancer related pain severe
- Weakness
- Poor nutrition
Plan:
- No further treatment of cancer in accord with patient’s instructions
- Pain Control: ibuprofen: 400 mg. every 4 hours, Oxycodone: 20 mg by mouth every 4 hours
- Nutritional counseling
- Have physical therapy evaluate for motion and activities of daily living
- Have occupational therapist evaluate for feeding and small muscle function
- Discharge note to primary care physician
Admit Note - Northeastern Regional Medial Center - Kirksville Missouri
2016 – Julia Morales
HPI
- Julia Morales, age 65, has lung cancer, which has been treated with chemotherapy and radiation, and now she wishes to stop treatment.
- Ms. Morales understands home hospice care; desires to die at home. She and her partner Lucy Gray are retired and have spent the past several years traveling together.
- Lucy is supportive of Julia’s decision and feels she will be able to care for Julia in their home. Lucy’s past medical history includes a knee replacement; some decrease in strength and mobility related to arthritis and past knee surgery. Their support system includes Julia’s son, Neil, and Lucy’s niece, Nora.
- Oncologist, Dr. Ann Davis in Columbia handing off care to hometown primary care physician Dr. King
- Oncology SW arranged for Kirksville OT and PT to assess home setting as Julia leaves hospital for home.
- Family physician Dr. King notified of OT and PT assessment which revealed distress at Julia/Lucy’s home as they tried to manage. Julia’s pain is not under control. Family physician admits Julia to hospital to allow the pain to be adequately & rapidly treated.
ROS
General: wt. loss, fatigue, weakness, lack of concentration/focus, night sweats, Ø fever, chills.
Integument: easy bruising, bleeding, positive for rashes, itching, thinning hair and sores; Ø lumps, moles, or nail changes,
HEENT: + for vision and hearing changes, headache, glasses. Ø tearing, itching or blurriness. Dry mouth/sore throat.
Pulmonary: SOB, non-productive cough, occasional hemoptysis. Ø wheezing
Cardiac: high blood pressure, angina, pitting edema, dyspnea on exertion; Ø Palpitations
GI: Decreased appetite, indigestion, dysphagia, nausea/vomiting, alternating constipation/ diarrhea, mouth sores; Ø abdominal pain, jaundice, hematechezia, hematemesis, melena, hemorrhoids.
Genital: postmenopausal, changes in libido, vaginal dryness; Ø itching, discharge, sores.
Urinary: urgency, occasional incontinence; Ø dysuria, frequency, hesitancy, hematuria.
Neuro: numbness and tingling; Ø tremors, fainting, blackouts, seizures.
Endocrine: cold/heat intolerance; Ø polydipsia, polyuria, polyphagia, excessive sweating.
Psychological: anxiety, increasing forgetfulness; Ø suicidal, homicidal ideation
PMH
Stage 4 adenocarcinoma of the lung diagnosed 4 years ago by bronchoscopy (right upper lobe). Received radiation and chemotherapy; Naturopathic treatment with aromatherapy oils and acupuncture
Past Surgical HX:
Hysterectomy at age 44
Family HX
Julia was married (divorced when son Neil was little); still talks to ex-husband.
Raised son Neil to adulthood by herself; Neil is now age 42 alive and healthy
Has been with partner Lucy Grey, age 73, for more than 25 years. While Lucy has a niece, Nora, Julia expresses concern about leaving Lucy alone.
Son Neil would like her to try more treatment, but even the doctor says there’s not much more they can do, besides keep her comfortable.
Social HX
College graduate/business degree; ran small nursery till age 50.
10 years smoking after college (1982)
Private insurance
Religion: Unitarian
Meds
Current meds:
- Stopping chemo
- Palliative or comfort care focus
- Phenergan 25mg by mouth every 4-6 hours for nausea/vomiting
- Vitamins and supplements for nutrition
- Oxycodone 20mg by mouth every 4 hours as needed for pain
- Ibuprofen 200mg by mouth every 4-6 hours as needed for pain
Allergies
No known allergies
Immunizations
Influenza and H1N1, last fall
Physical Exam:
Race: Caucasian
Weight: 113 lbs
Height: 64 inches
-BP: 152/94, P. 82 and regular, R. 24 and slightly labored, T. 98.2F, BMI=19.4
General: appears ill, poorly nourished; alert and oriented x 3,
Scalp: atraumatic, hair normal pattern, texture and distribution
Eyes: PERRLA, fundi without AV nicking or exudates, Ø obvious papilledema
Ears: EACs clear, atraumatic, TMs pearly grey, translucent, hearing grossly intact to voice and whisper
Nose: nares patent bilaterally, septum intact, Ø discharge, polyps or bleeding
Mouth: Edentulous with upper and lower dentures, white patches inside cheeks, pharynx non-erythematous without exudate, uvula midline
Throat: No erythema, exudate. Tonsils normal.
Neck: supple, full and non-tender ROM, Ø bruits, lymphadenopathy, thyromegaly
Chest: symmetric and non-tender with normal AP diameter, erythematous areas from radiation therapy
Lungs: auscultation bilaterally reveals coarse rhonchi and area of decreased breath sounds on right upper lobe
Heart: rate and rhythm regular, Ø murmurs, rubs or gallops
Abdomen: Soft and non-tender, bowel sounds normoactive, Ø hepatosplenomegaly
GU: deferred
BACK: Full ROM, Ø spinal tenderness, CVA tenderness
EXTS: upper and lower extremities with grossly full ROM. Pulses 4+ and equal bilaterally. Ø joint swelling or calf tenderness. General weakness.
OSTEOPATHIC MUSCULOSKELETAL EXAMINATION:
Performed in seated and supine positions; increased thoracic kyphosis; mild scoliosis.
Tissue texture abnormalities, asymmetry and restricted motion, with some tenderness in the cervical, thoracic, ribs, lumbar, sacral, pelvic and abdominal regions.
Major somatic dysfunctions: bilateral para-spinal tightness and muscle spasms in the cervical, thoracic and lumbar spine; T3 FRLSL, T5-7 NRLSR, T9 ERRSR, R Ribs 3-5 exhaled, L Ribs 6-8 inhaled, L5 ERLSL, R sacral torsion, R anterior innominate; restriction in celiac ganglion, superior mesenteric ganglion, and inferior mesenteric ganglion
Major correlations: viscerosomatic, primarily musculoskeletal, pulmonary, and gastrointestinal
Impression:
- Terminal cancer, small cell lung cancer in right upper lobe
- Pain secondary to terminal cancer
- Oral candidiasis
- Hypertension vs reactive blood pressure due to lack of pain control
- Somatic dysfunction in C/T/R/L/S/P/A.
Plan:
- Admit with referral to pain management team
- Continue oxygen
- Plan for discharge to home with hospice care
- Assess for cognitive status and depression;
- Spiritual and emotional assessment
- Psychology consult
- Based on today’s physical exam findings, OMM was performed and was well-tolerated. Techniques used included muscle energy, BLT, myofascial release, HVLA, and soft tissue. Treated areas include cervical, thoracic, ribs, lumbar, sacral, pelvis, and abdomen.
Occupational Therapy
Patient Name: Morales, Julia
Reason For This Admission: Home Safety Eval/Home Health
PMH: Pt has no hx of prior OT. Pt is being seen due to recent dc to home following tx in Columbia for stage 4 lung CA with possible brain and bone mets.
S: “Sorry it took me so long to get to the door”, “The therapist was already here today.” “What do you do?” “I am so tired….sometimes I wish I would fall asleep and just not wake back up…it would be easier on Lucy and Neil if that’s how it happened.”
O: OTR reviewed pts past HX prior to visit. OTR explained the purpose of OT, pt then verbalized understanding and was willing to accept tx. Pt took a long time to get to the door. Home is strewn with piles of unrelated objects, mail, newspapers, and the kitchen is very cluttered with jars of multiple supplements and herbs which interfere with food prep areas. Pt used FWW for ambulation. Home is 2 story with bedrooms upstairs and a half bath on the ground floor. Pt is on O2 at 2l. per nasal prong. Pt is SOB with minimal exertion and O2 dropped from 94% to 88 % following 20 ft walk from living room where she has been sleeping on a fold out sofaabed to the bathroom aprox 20 ft down the hall and stopped 4x on the way to catch her breath. Bathroom contains no adaptive equipment. The O2 concentrator is in the same closet with the cat litterbox and there is a strong odor of cat urine/feces throughout the home. Pt c/o prbs getting dressed, bathing, meal prep, and getting up and down from the toilet due to pain and SOB. During eval, Lucy, the partner arrived home with bags of items from the store and Goodwill. She complained that even though the nosy neighbor next door could see her struggle, there was no offer of help. OTR attempted to engage her in discussion of Julia’s needs but she claimed she had too much to do and felt overwhelmed. Son, Neil called during eval and could be heard speaking loudly to Julia, warning her to be careful with the new walker. He promised to come by after work.
OT eval reveals:
- BP=160/88, P=88, R=20, Temp=98.4, Pain=5 in middle of back and neck.
- Pt denies prbs with chewing, choking, swallowing. She c/o decreased appetite
- Pt requires SBA to MIN A to arise from surfaces but is steady but SOB during ambulation.
- Pt wears bifocals. Lucy complains that Julia is not hearing well but does not have hearing aids.
- Pt has dentures and is experiencing some problems with them not fitting, and some sensitivity .
- UE ROM is WFL, UE Strength is F +. Thoughout., Cardiovascular endurance is low and does not allow for typical ADL.
- Bed mobility is poor, partly due to the soft mattress on the pull out sofa.
- Pt tolerated 5 min standing meal prep at kitchen counter before pain and fatigue required her to sit. Pt c/p pain of “6” and added that she “didn’t realize just how much energy it take to do regular things’. Lucy attempted to finish the food prep and bring it to the table but had evidence of pain herself.
- Pt said she likes to travel, play with the cats, read, watch baseball on TV with Lucy, watch the birds and cook for fun. She misses Lucy’s niece Nora and the fun visits they used to have back before she became a nurse.
Tx today: OTR advised pt to avoid storing O2 concentrator in a closet or near anything that would contaminate the air. Pt was advised to wash the filter weekly and she admitted she did not even know there was a filter. OTR recommended obtaining a bath chair that could be used in front of the the sink since there is no tub or shower available on the first floor. The kitchen sink would actually be a better alternative but that area is too cluttered to be safe. Pt was agreeable to these recommendations. By the end of the session she was laughing and joking about how her cats will find her dead one day, but will probably just step over her on their way to the litterbox until the smell gets too bad to handle. Then they will all go to Paris together and with all their 9 lives will have time to travel all over the world to the rest of the places Julia and Lucy never got around to going to. Lucy overheard this and scolded Julia and told her it was “nothing to joke about”.
A: The following problems will be addressed by OT:
- Decreased endurance, pain, and cluttered environment interfere with safe, routine ADL such as bathing, dressing and meal prep
- Knowledge deficit regarding safe and effective use of o2 creates risk of falls
GOALS:
1.
- a. Pt will ambulate 20 ft to bathroom, perform brief sponge bath at sink with bath chair with min SOB and pain less than 5, with min caregiver assist within 2 weeks
- b. Pt will tolerate very light meal prep with mod a.
- c. Pt will dress and undress with min-mod A.
2. Pt will demonstrate safe use of O2 and be free of falls. Pt will demo ability to turn on O2 concentrator, adjust liters per dr recommendation, manage tubing during ambulation.
P:
- ADL training in areas of bathing, dressing and meal prep while using O2. Will assess frequently for pain and SOB
- Adaptive equipment recommendations and training
- Safety training re use of o2 and energy conservation, positioning and breath control.
- Request MSW eval due to pts statements about not wanting to wake up and to explore possible support/counseling regarding the condition of the home
DC Plan: OT 3x a week x 3 weeks and DC to ongoing Hospice care at home. Pt will likely require a home health aide on a continuous basis as her condition worsens. Will train HHA in above skills as needed depending on Lucy’s ability and willingness to help with ADL
Lizette Touche, , OTD, OTR/L 9/23/16, 1530.
Social Work
INITIAL SOCIAL WORK ASSESSMENT
Patient Information
Patient is a 65 year old female diagnosed with lung cancer 4 years ago. Pt. decided to discontinue cancer treatment stating, “nothing good came out of it.” Pt goes on to say that it “hurts to breath” that she is “losing strength” and that she is “just ready to let things happen naturally.” Patient was recently discharged home from an oncology center in Columbia, Mo. only to be admitted to the hospital 2 days later for pain management. Patient reports that her partner of 25 years, Lucy, is having a hard time coping with having to be in a caregiver role.
Financial Information
Patient receives $1500.00 monthly from Social Security and has Medicare for health insurance. She has a “small” amount of money in a retirement fund. She is the sole owner of her home and owns it outright. Patient expressed that she did not want to discuss anything further in front of her son, Neil.
Dental/Oral Health
Patient reports she has sores in her mouth making it difficult to eat.
Physical Health
Patient reports she has lost a significant amount of weight, is in constant pain, and has been losing strength over the last 6 months. She reports she can walk short distances, however, cannot climb the stairs in her home. She adds that this impairs her ability to access the bathroom located on the second floor. Patient reports using the half bathroom downstairs is her only alternative. The patient asserts that despite all these difficulties, her desire is to die at home.
Mental Health
When asked about the status of her mental health, the patient reported that she sometimes feels low and depressed. She discussed how overwhelmed she feels about leaving her family behind and how she is “just plain tired.” She explains that all the running around to get treatment has really “taken its toll.” She adds that sometimes she wishes that she could just go to sleep and not wake up. When asked if she ever thinks about ending her life the patient firmly states “no.” She adds “I could never do that to my family. I will just wait until my time comes naturally.”
Family/Social Support System
The patient identifies her partner of 25 years, Lucy, her son Neil, and Lucy’s niece Nora as her primary sources of support. All three were present and were given an opportunity to participate in the assessment. Lucy reports that she feels very overwhelmed by the patient’s decision to end cancer treatment. She noted that she feels as though she were left out of the decision making and often feels “low” and “nervous” about the future. Furthermore, she reports that she is not able to make decisions very well, and is having a hard time coping with her caregiver responsibilities. She admits that the patient was the “strong” one in the relationship and that she often relied on the patient. She adds that although she very much wants to help the patient with her care needs, she is limited due her history of knee replacement surgery and consequent instability. She acknowledges that her relationship with Neil is strained due to her “saving” behavior and admits that the set-up of the home could pose a risk to the patient.
Neil reports his own experience of sadness regarding losing the “only family member” he has. He reports a deep love and respect for his mother and wishes she would keep on fighting. When asked, he notes that his relationship with Lucy is a good one. He states that he has no animosity against her, but cannot be responsible for Lucy’s well-being after his mother passes. His concerns include the safety of the home environment, Lucy’s physical ability to carry out caregiving responsibilities, and how Lucy will be able to take care of herself both physically and financially once his mother passes. He discusses the financial concerns at length explaining that his mother is the sole owner of the home and questions, “who will be the owner of the home?” He is also concerned about how Lucy will manage financially as her Social Security is much less and she has not retirement account. He goes on to say that his time is very limited and that he lives far away. He expresses a desire to be helpful, but states that his job is very consuming and that he cannot give what he does not have.
Nora adds to the list of concerns stating that the patient is sleeping on a fold out couch and does not have adequate access to a full bathroom. She agrees that the home is not safe due to “cats and clutter” and questions whether hospice services can be set up in the home. Nora discusses her concerns regarding how the patient and her partner will manage tasks like food shopping and cooking as there has already been some difficulty with this in the recent past. Nora is willing to help where and when she can.
Transportation
The patient historically has been the primary driver in the relationship. She reports that although she “can still drive” she is concerned about how much longer she can do this as she “gets weaker” every day.
Psychosocial Assessment Summary
S/O - The patient is a 65 year old female being referred to social services to evaluate for discharge planning needs. The patient and her partner wish for the patient to be cared for in their home. The patient’s partner reports some difficulty due to her own medical history, however, very much wants to honor the patient’s wishes. The patient’s support system seems to disagree noting the home to be unsafe for a variety of reasons including “cats and clutter,” limited accessibility to a bathroom, and inadequate sleeping arrangements for the patient.
A - The patient’s desire to be cared for at home may be unrealistic due to a possible unsafe home environment, limitations of her caregiver’s capabilities, and a less than adequate support system. There also seems to be some financial concerns regarding the patient’s assets and how her surviving partner will manage after she passes. The family dynamic appears mostly functional, yet strained at the same time. There seems to be some strife between the patient’s partner and her son, yet they both care very deeply for the patient. This is possibly common ground from which they can both establish goals for how the patient should be cared for. The partner’s niece appears to be willing and able to a source of support and help. Although the patient verbalized not wanting to wake up, she denies any suicidal ideation or intent.
P
1. Present options to return home as the patient wishes. Offer alternatives in the event returning home proves unsafe.
2. Address the patient’s caregiving needs by referral to community resources.
3. Present community referral information to address legal concerns.
4. Solution-focused family counseling to establish common goals for how the patient is to be cared for until the time of her passing.
Assessment Completed By:
Will B. Helpful, MSW, LCSW
Northeast Regional Medical Center
9/24/2016
SOCIAL WORK DISCHARGE NOTE
S/O - Met with patient and extended family and engaged in solution focused family counseling. Dicussed discharge planning options. Patient and family reiterate their wishes that the patient be returned home. Discussed implications of clutter in the home and the limitations that the patient’s partner has with caregiving. Also discussed concerns regarding legal matters such as the absence of advanced directives, health care power of attorney, and matters related to the patient’s property and estate planning.
A - The patient’s only wish is to be returned home and she is likely to resist any other option at this time. Based on patient-centered care, the patient should be returned home with multiple supports in place to address the following needs:
- Safe arrangement of home
- Caregiver support/assistance
- Food preparation and nutrition needs
- Access to adaptive equipment
- Advanced Directives
- Health Care Power of Attorney
- Estate planning
- Provision for surviving life partner
P - Refer to Hospice Compassus in Macon, Missouri to address home care needs. Refer to R. Timothy Bickhaus, Attorney at Law in Macon, Missouri to address legal needs.
Discharge Note Completed By,
Will B. Helpful, MSW
9/25/2016
Nursing
Nursing Discharge Summary - Columbia Hospital
Julia Morales, age 65 years, a patient at Columbia Hospital in Columbia, MO, was discharged on 9/22/16 following several days of hospitalization for lung cancer, chemotherapy, and radiation. She wishes to stop treatment. During her hospitalization, the nursing staff provided pain management for severe pain; nutritional support for her nausea and weight loss; assessment of respiratory status with oxygen therapy provided prn by nasal cannula; patient and caregiver education for ambulation and pain management; patient education and treatment for constipation or diarrhea. Nursing staff instructed patient and caregiver about pain management, medication administration, nutrition, ambulation, and exercise. Caregiver (Lucy) expressed concerns about patient’s significant needs and caregiver’s ability to provide care to meet patient’s needs. Summary of the patient’s plan of care was provided to caregivers. Physicians, Dr. Ann Davis (oncology) and Dr. King (family physician in La Plata) communicated regarding a discharge plan for OT and PT home assessment in patient’s home town of La Plata, MO. Phone contact made for OT and PT assessment of home setting. OT and PT agreed to visit home for assessment and determine appropriateness of care at home.
Sandra Smith, RN, BSN
Discharge Planning, Columbia Hospital
Sept. 22, 2016
NURSING Documentation - Northeast Regional Medical Center
Physical Therapy
Patient Name: Julia Morales
Age: 65
Language: English
Referral Source: Columbia Hospital
Date of Report: September 23, 2016
Reason For Referral: Physical therapy exam and treatment to assess mobility and transfers, need for adapted equipment, and caregiver training.
History: Julia is a 65 year old female with a history of Stage IV lung cancer. She has been undergoing treatment for the past four years which includes radiation and chemotherapy as well as naturopathic treatments. Julia has been referred to Hospice for palliative care.
Social History: Patient lives with 73 year old partner and five cats in her two story home.
Prior Level of Function: Prior to onset of current condition 4 years ago, patient was independent in mobility, self-care and was active, often traveling out of country. In the past few months she has maintained independent ambulation, and needs help getting from bed to standing. She states she is limited by fatigue, pain and shortness of breath.
Home Environment and Resources: Patient lives in a two story home with bedrooms and full bath upstairs, ½ bath (sink and toilet) downstairs. Julia has been sleeping on a fold-out couch in the living room.
S: Patient is concerned about pain, fatigue and being a burden to care for. Patient’s partner is concerned about being able to help patient with medications for pain, and helping her move within the home.
Patient’s Goals: Patient would like to be able to move throughout her home, sit in the backyard or enclosed porch to visit with friends and family and view her garden. She would like to decrease her pain and help in self-care as much as possible.
O:
REVIEW OF SYSTEMS
Cognition: Patient is alert and oriented x4.
Respiratory: Breathing is fast and shallow.
Integumentary: Fingernail clubbing bilaterally with slightly cyanotic nail beds. Skin is ashen in color. Visual exam of skin on arms, legs, back and buttock reveals no skin breakdown.
Musculoskeletal: Gross muscle exam performed. Strength is 3/5 throughout. Patient has no significant limitations in active range of motion of upper or lower extremities.
TESTS AND MEASURES
Vital Signs: Temp is 97.6° F; HR is 92 bpm, BP is 156/90. Respiratory rate (with 2L 02) 20 breaths/minute at rest. Increased to 25 breaths/min with ambulation. SpO2 is 92% at rest, and 86% with ambulation.
Balance: Scored 25 out of 56 on the Berg Balance Scale (medium fall risk)
Transfers: Supine - sit minimal assist of 1; sit - stand (from fold-out bed) moderate assist of 1 without assistive device. With walker, required minimal assist of 1.
Gait: Patient ambulates unsteadily and prefers to hold onto partner, walls or furniture. Gait velocity is slow at 0.4 m/s (12 seconds to walk 5 meters). Patient was assessed using front wheeled walker (brought by PT) and was modified independent ambulating using the front wheeled walker in the kitchen. Patient initially had difficulty managing the oxygen tubing along with the walker but was safe by end of session. Unable to ambulate using the front wheeled walker in living room or bathroom due to stored collectibles. Patient declined stairs due to fatigue.
Endurance: Will perform 2-Minute Walk Test once collectibles have been cleared to allow test to be performed.
Pain: Pain is currently 6/10 on visual analog scale, however patient reports this varies throughout the day
Home Accessibility: Patient lives in two story home with 7 steps to enter home. Kitchen, living room, ½ bath, and front porch are accessible to patient. Home is filled with collectibles which create narrow pathways through living room and kitchen. Patient’s cats are attracted to oxygen hose, and were observed to play with the hose as patient ambulated, which may pose a hazard.
Caregiver Training: Patient’s partner was instructed in transfer assistance. Able to help with supine - sit; Unable to help with sit - stand safely, stating “knees are weak and painful”.
Assessment: Limitations in transfers and mobility; at risk for skin breakdown due to prolonged bedrest and sitting. Limited by pain and poor endurance.
Recommendations:
- In addition to the front wheeled walker, patient would also benefit from a as wheelchair in the home to meet goal of household mobility. Home will need to be modified (collectibles rearranged) to allow access to walker and wheelchair.
- Instruct patient in energy conservation techniques
- Transfer training, especially supine - sit and sit - stand
- Caregiver training
- Monitor oxygen saturation with activity
- Pain management, including teaching patient diaphragmatic breathing, biofeedback, imagery
Goals:
- Patient will ambulate with modified independence using front wheel walker and managing oxygen tubing throughout the downstairs and patio with 2 L O2 and maintaining oxygen saturation above 88%.
- Patient will be modified independent with wheelchair mobility within the first floor of her home and on patio.
- Patient will transfer supine to sit and sit to stand with modified independence.
- Patient’s caregiver will independent and safely assist patient with transfers, when patient is fatigued and needs extra help.
- Patient will verbalize and incorporate energy conservation techniques during activities of daily living.
- Patient will be independent with pain management techniques (diaphragmatic breathing, biofeedback, imagery) to allow patient to better manage her pain.
Plan: PT 3x/week for 3 weeks then discharge to ongoing hospice care at home.
Myrna Stipovic, PT, DPT MO license #3678
Health Educator
Health Educator/Health Education Specialist NOTES
What is a Health Education Specialist/Health Educator?
The U.S. Department of Labor – Bureau of Labor Statistics (BLS) has a classification of health educator and defines health educators (SOC 21-1091.00) as those that provide and manage health education programs that help individuals, families, and their communities maximize and maintain healthy lifestyles. Health Educators collect and analyze data to identify community needs prior to planning, implementing, monitoring, and evaluating programs designed to encourage healthy lifestyles, policies, and environments. They may serve as resource to assist individuals, other health professionals, or the community, and may administer fiscal resources for health education programs. Excludes “Community Health Workers” (21-1094).
- According to the U.S. Department of Labor (DOL), there were an estimated 58,900 health educators in 2012.
- Employment of health educators will grow by projected to grow 21 percent from 2012 to 2022, faster than the average for all occupations.
- 5 out of 10 health educators work in healthcare and social assistance
- 2 out of 10 work in state and local government
LINK: http://www.bls.gov/oes/current/oes211091.htm
Health Education Specialists prevent disease, promote health, and keep communities safe through Seven Areas of Responsibility:
Area I: Assess Needs, Resources and Capacity for Health Education/Promotion
Area II: Plan Health Education/Promotion
Area III: Implement Health Education/Promotion
Area IV: Conduct Evaluation and Research Related to Health Education/Promotion
Area V: Administer and Manage Health Education/Promotion
Area VI: Serve as a Health Education/Promotion Resource Person
Area VII. Communicate, Promote, and Advocate for Health, Health Education/Promotion, and the Profession
LINK: Areas of Responsibility for Health Education Specialists 2015
HEALTH EDUCATION SPECIALIST PROVIDES ‘HEALTH EDUCATION/RESOURCES’ FOR THE PATIENT/FAMILY:
- THE HEALTH EDUCATION SPECIALIST WILL EDUCATE THE PATIENT AND FAMILY ABOUT ADVANCED CARE PLANNING http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3277
http://www.caringinfo.org/files/public/ad/Missouri.pdf
- THE HEALTH EDUCATION SPECIALIST WILL EDUCATE THE PATIENT AND FAMILY ON SETTINGS FOR HOSPICE/PALLIATIVE CARE – HOME HEALTH, SKILLED NURSING, HOSPITAL
http://health.mo.gov/safety/homecare/, health.mo.gov/safety/showmelongtermcare/ppt/HospiceCare.ppt, https://www.mohospice.org/, http://www.aafp.org/afp/1998/0201/p491.html, http://www.nhpco.org/sites/default/files/public/regulatory/Criteria_for_General_Inpatient.pdf
- Talking to the family about how to choose a hospice- THE HEALTH EDUCATION SPECIALIST WILL TAKE THE FAMILY THRU THE LIST OF QUESTIONS:
http://moments.nhpco.org/sites/default/files/public/moments/Choosing%20a%20Hospice.pdf ; http://www.nhpco.org/about/hospice-care
- THE HEALTH EDUCATION SPECIALIST WILL ALSO EDUCATE THE FAMILY ABOUT GRIEF AND LOSS:
http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3367
- THE HEALTH EDUCATION SPECIALIST WILL EDUCATE THE FAMILY ABOUT ‘CAREGIVING’ -
http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3323
Patient-Family Resources: Lung Cancer
http://www.cancer.gov/types/lung ;
Education - Hospice/Palliative care
- Hospice care is end-of-life care. A team of health care professionals and volunteers provides it. They give medical, psychological, and spiritual support. The goal of the care is to help people who are dying have peace, comfort, and dignity. The caregivers try to control pain and other symptoms so a person can remain as alert and comfortable as possible. Hospice programs also provide services to support a patient’s family. Usually, a hospice patient is expected to live 6 months or less. Hospice care can take place •At home •At a hospice center •In a hospital •In a skilled nursing facility (NIH: National Cancer Institute)
- Palliative care - When you are facing a serious illness, you need relief from symptoms. You need to better understand your condition and choices for care. You need to improve your ability to tolerate medical treatments. And, you and your family need to be able to carry on with everyday life. This is what palliative care can do - https://getpalliativecare.org/whatis/
- Hospice USDHSS: http://www.eldercare.gov/ELDERCARE.NET/Public/Resources/Factsheets/Hospice_Care.aspx
a. Hospice in Missouri: http://health.mo.gov/safety/hospice/index.php
Patient/Family Resources – Hospice/Palliative care
Handouts/Organizations - https://medlineplus.gov/ency/patientinstructions/000467.htm, http://hpna.advancingexpertcare.org/wp-content/uploads/2015/04/PT04E-Final-Days.pdf, http://www.nhpco.org/, http://www.caringinfo.org/i4a/pages/index.cfm?pageid=1 http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3454 http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3406
Palliative care - http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3355 , https://getpalliativecare.org/ ; http://www.caringinfo.org/i4a/pages/index.cfm?pageid=3343;
Clinical Trials/research - https://clinicaltrials.gov/search/open/intervention=%22Hospice+Care%22 ; http://www.nhpco.org/research
Providers in the area - https://netforum.nhpco.org/eWeb/DynamicPage.aspx?Site=NHPCO&WebKey=a9338cdd-546a-42f5-9061-6b91dbdb31da; http://www.hospicedirectory.org/cm/search ; https://getpalliativecare.org/providers/missouri/ https://www.agingcare.com/local/hospice/kirksville-mo https://www.agingcare.com/local/Hospice-2000-DBA-Hospice-of-Northeast-Missouri-Kirksville-Hospice-MO
Dental
Comprehensive Dental Exam
S:
Julia Morales, age 65, has lung cancer, which has been treated with chemotherapy and radiation, and now she has stopped treatment.
CC: “Loose denture and burning mouth”
Med HX:
Stage 4 adenocarcinoma of the lung diagnosed 4 years ago by bronchoscopy (right upper lobe). Received radiation and chemotherapy. Naturopathic treatment with aromatherapy oils and acupuncture.
wt. loss, fatigue, weakness, lack of concentration/focus.
high blood pressure, angina, pitting edema, dyspnea on exertion
Hysterectomy at age 44
Allergies: NKDA
Medication HX:
- Stopping chemo
- Palliative or comfort care focus
- Phenergan 25mg by mouth every 4-6 hours for nausea/vomiting
- Vitamins and supplements for nutrition
- Oxycodone 20mg by mouth every 4 hours as needed for pain
- Ibuprofen 200mg by mouth every 4-6 hours as needed for pain
Social Hx:
College graduate/business degree; ran small nursery till age 50.
10 years smoking after college (1982
Religion: Unitarian
Dental Hx:
Pt has dental phobia. according to her this is the reason she lost most of her teeth. MX. Upper denture is only 4 years old but it is loose now. Pt reports that denture and partial denture do not fit well. Pt is satisfied with the look of her teeth. Pt has trouble chewing food bc denture “clicks” or comes loose while chewing. Pt reports slight sensitivity in lower L posterior occasionally, no pain. Pt doesn’t remember having a dental cleaning.
O:
BP: 133/91 mmHg P: 69 bpm
Blood sugar: 145 mg/dL
Clinical Exam:
EOE: WNL
IOE: Bilateral bone depression between ridge and RMP. Redness under denture along with some white patches. Redness around the corner of the mouth.
TMJ: R pop upon opening
OSC: Negative
Hard Tissue:
Pt has full upper denture
Lower has FPD on lower with 29, 27, 23, 22, & 20 as retainer teeth
20: recession, check after SRP
22: check after SRP
23: check after SRP
27: recession, check after SRP
29: check after SRP
Teeth seem sound, but recheck margins of crowns after cleaning
A:
Candidiasis / Angular cheilitis
Perio Dx: Generalized chronic periodontitis
Perio Risk: moderate due to long-span bridge forces
Caries risk: high due to dry mouth
OC risk: high due to smoking
Speech & Language Pathology
Initial Evaluation and Discharge Note: clinical examination of dysphagia
Patient Name: Julia Morales
Reason For This Admission: small cell lung cancer
Reason For Referral: OT noted chewing, choking, swallowing problems
S: Patient was admitted for chemoradiation treatment for lung CA.
Today she is seen while sitting upright in a chair, alert and oriented x3, and able to communicate her concerns and describe the chewing/swallowing problems she is experiencing. Staff noticed reduced hearing and she concurs and believes the change is a side-effect of the chemotherapy as was noted as a risk. In the quiet of her room and maintaining her attention, face-to-face conversation was not difficult. Intermittently, intentional comments were made when not face-to-face to test her ability to follow comments and there was a definite change in comprehension.
She is edentulous with dentures. Apparently before the treatments for lung cancer her dentures fit well and she was able to eat all textures with ease. With weight loss associated with treatments she has noted a gradual change in how the dentures fit, and it has gotten to a point where the poor fit interferes with chewing. In addition, especially noted after the last “couple” chemotherapy treatments, she has developed sores in her mouth. Candidiasis has been diagnosed. The ill-fitting dentures and mouth sores combined pose difficulty in chewing. She also reports coughing, but does not associate coughing with choking. Rather, a component of the lung cancer.
There are numerous references in her chart indicating oxygen de-saturation with exertion.
O:
Swallowing assessment was completed via administration of the Mann Assessment of Swallowing Ability (MASA) and food observations were completed at the same time with her lunch, using food from her meal.
Inspection of the oral cavity revealed small sores on the gums, tongue, and buccal lining as well as erythema and edema of these same sites. One spot of exudate was noted. Lip seal, tongue movement, and tongue strength were mildly reduced. Voice was clear. Laryngeal elevation appeared timely with full excursion as judged by finger palpation.
Functional implications were to the oral phase of deglutition where chewing was careful, slow, and labored and oral transit of bolus was slow. At rest oxygen saturation was steady between 93 and 95% and while chewing a decrement in saturation was noted to between 88 and 90% when shortness of breath was also observed. A planned pause between bites facilitated return of saturation to 91 and 92% and shortness of breath was reduced as a consequence. No coughing was noted during the examination. She avoided the hard, crunchy foods that were provided with her meal, eating only soft foods. Upon query the patient indicated that she preferred the applesauce that was provided, as it was easier to swallow and its cool temperature was soothing to her mouth. She indicated a willingness to eat a combination of very soft foods combined with ground meats while her mouth healed.
A: Total score on the MASA was 180, indicating possible dysphagia. Signs and symptoms related to the oral phase and some alterations in function occurred in conjunction with facial grimace and verbalized discomfort while chewing and manipulating the bolus. There were no signs of aspiration while eating.
P:
- Recommend that the Patient be placed on a modified diet with soft textured solids and ground meat to reduce pain associated with chewing and while awaiting healing of sores in mouth and evidence of response to treatment of candidiases. Temperature extremes and spicy foods should be avoided, as well.
- Referral to dentistry for adjustment of dentures.
- Referral to audiology for hearing
- Additional need for speech pathology services is not required at present as the patient expressed understanding of the situation and the recommendations and indicated a willingness to follow them. She also understands that healing is anticipated and she can re-introduce foods as pain diminishes.
Katherine Janeway, M.A., CCC/SLP
Certified Athletic Trainer
Consultation: Certified Athletic Trainer Notes
Certified Athletic Trainers – Job Description:
An Athletic Trainer is an allied health professional who, under the supervision of a physician, is an integral part of the health care system. The athletic trainer provides a variety of medical services including injury prevention, injury treatment including immediate care, injury recognition, and rehabilitation techniques of injuries. Athletic Trainers work with physically active people. Their education and expertise allows them to clinically diagnose injuries, administer emergency treatment, determine if specialized medical care is required, rehabilitate injuries, and advise on appropriate equipment beyond those related to athletes. Athletic Trainers work in a variety of settings including, but not limited to, colleges and universities, high schools, rehabilitation facilities, corporate offices, professional dance and theater groups, sales, gyms, Nascar, professional athletics, rodeos, military, occupational health, and hospitals.
Professional Domains
Athletic Trainers are educated to provide comprehensive patient care in five domains of clinical practice.
- Prevention
- Clinical evaluation and diagnosis
- Immediate and emergency care
- Treatment and rehabilitation
- Organization and professional health and well-being
Clinical Learning
Athletic Trainers pass competencies in clinical learning to prepare them to possess the skills and clinical abilities along with a broad scope of foundational behaviors of professional practice.
- Evidence-based practice
- Prevention and health promotion
- Clinical examination and diagnosis
- Acute care of injury and illness
- Therapeutic interventions
- Psychosocial strategies and referral
- Health care administration
- Professional development and responsibility
CCCC Athletic Training Notes
Patient 1
Can refer/find information regarding hospice care
Recognize mental health issues and understand referral strategies
Provide lung and chest strengthening exercises through breathing techniques
Provide simple exercises to maintain cardiovascular and muscle tone (in home exercises that can use what is already available)
Patient 2
Knee exercises – clinic and home programs, pool program could be beneficial
Proper use of cane
Walking exercises
Monitoring for infection and adverse effects
Provide simple exercises to maintain cardiovascular and muscle tone (in home exercises that can use what is already available)
Monitor for blood clots (DVT) in leg and provide patient education of what to look for
Both
Encourage to attend follow up appointments – suggest methods to travel if appropriate
Provide strategies for living situation changes (moving bedrooms downstairs)
Possibly a chair lift/elevator to go up and down the stairs
Recliner that helps to lift to stand
Medical bed brought into house
Assessing for home safety
Suggesting community support groups for both women and family members
Pharmacological education – proper use of medication and storage
Monitor for blood clots in leg and provide patient education of what to look for
