Henry’s Hospital Stay
 History of Present Illness:
History of Present Illness:
Henry was admitted to Poplar Bluff Regional Medical Center with an acute exacerbation of COPD. He was not able to catch his breath and his primary care doctor told him to go to the emergency room. His neighbor brought Henry and his wife to the emergency room. Henry is concerned about his wife, Ertha, who has problems with memory and seems confused at times.
His daughter-in-law Betty is a nurse. She mentioned that Henry appears depressed because his appetite has diminished over the past 2 months and he has lost some weight. He has also lost interest in his previous activities such as following major league football and working on crossword puzzles. Betty has been looking after Ertha while Henry is in hospital.
Some additional thoughts from Henry and Ertha while Henry is in hospital.
Case Notes
Nursing
Nursing Plan of Care
Nursing Diagnoses |
Nursing Outcomes |
Nursing Interventions |
Care Plan Discharge Evaluation |
|
Impaired Gas Exchange secondary to exacerbation of COPD. Ineffective Airway Clearance. |
Respiratory Status: Maintain at >88% at 2 liters of O2 by nasal cannula. Maintain at 3 (moderate deviation from normal). Demonstrate effective coughing and clear breath sounds. |
Respiratory monitoring: Monitor rate, rhythm, depth, and effort of respirations. Administer oxygen as ordered to maintain O2 sat as ordered. Administer Nebulizer treatment as ordered. Education: Provide education about effective controlled coughing. Encourage deep breathing and use of Incentive Spirometry as ordered. |
3 - Respiratory Status: Clients O2 saturation was maintained above 88% with continual O2 therapy. Client demonstrated effective coughing. Sputum clear and decreasing amounts. Client demonstrated effective coughing and purse lipped breathing technique. |
|
Activity Intolerance. |
Endurance: Maintain at 3 (moderately compromised). Energy Conservation: Balances activity and rest. Maintain at 3 (sometimes demonstrated). |
Activity Intolerance: Energy management, exercise promotion, self-care assistance. Assist with transfers and ambulation. Request and order for consultation with Physical Therapy if indicated. |
3. Client able to ambulate to bathroom with assistive device. Ambulate in hallway 150 feet with slow gait and no distress. Tolerating sitting in chair for meals and 30 minutes TID. Transfers independently with assistive device. States feeling stronger. PT consultation and therapy completed. |
|
Imbalanced Nutrition: food intake less than RDA. |
Nutrition: Will consume adequate nutrition. Maintain at 3 (moderately compromised). |
Assess diet compliance, needs, barriers. Request order for Nutrition consultation if indicated. Allow rest periods during meals. Assist patient to sit up in bedside chair for meals. |
3- Moderately compromised. Dietary consultation completed. Education regarding COPD diet complete. |
|
Readiness for Enhanced self-health management related willingness to consider smoking cessation. |
Smoking cessation behavior: 4-5 (often demonstrated/consistently demonstrated). |
Assess barriers to smoking cessation and brain storm solutions with client and family. Provide smoking cessation information and support. |
5- Consistently demonstrated. Client verbalizes desire to quit smoking. Strategies identified and employed. |
|
Anxiety |
Anxiety Level: Verbalized anxiety. Maintain at 3 (moderate). |
Anxiety reduction: Use calm, reassuring approach. Clearly state expectations for patient’s behavior. Identify when level of anxiety changes. Listen attentively. Create an atmosphere to facilitate trust. Assess support systems. |
3-4 Moderate anxiety level. Patient’s goal rating is a 4. Social work consultation done. |
|
Risk for depression. |
Depression Level: Depressed mood. Increase from 3 (moderate) to 2 (mild). |
Coping enhancement: Appraise the patient’s understanding of the disease process; appraise the patient’s needs/desires for social support. |
3- not met. Geriatric depression scale (short from) completed and scored 6. Reported to attending physician. Will f/up out patient. |
|
Caregiver role strain |
Family Coping: Manages family problems. Increase from 2 (rarely demonstrated) to 3 (sometimes demonstrated). |
Caregiver support. Family support. Counseling. Referral. Environmental management: home preparation: Assess home needs concerning preparation for care delivery at home. Consult Home Health, Social Services, etc. as indicated. Mutual goal setting: Identify with patient the goals for care; explore with patient ways to best achieve goals. |
3- goal met. Plan for caregiver support initiated. Will need to monitor ability to follow through after discharge. Social Service, discharge planning initiated on admission and complete. Patient to discharge to IP Rehabilitation Unit. |
NURSING NOTES
Day 1Day 1: Admission notes: Vital signs upon admission: T=99.2 oral, P=92, R= 30, BP=130/82. O2 sat 92 on 4 L/NC. Admitted to the unit from ER accompanied by his wife. Patient stated, “I am so out of breath and weak as a cat!” Assisted patient from wheelchair to bed and he stated he “felt dizzy”. Noted his gait was unsteady. O2 at 4 liters/minute by nasal cannula. O2 sat at 88% after transfer from WC to bed. Note physician order for O2 at 4 liters/NC to maintain sat at 92%. HOB elevated. Assisted patient to rest leaning forward over the “over the bed table”. Instructed patient on pursed lip breathing. O2 sat 92%, breathing easier, respiratory rate 24. Patient states that over the past three days he has become “very short of breath with any walking and unable to go far”. Patient relates that he also “gets very short of breath when he tries to eat.” Patient demonstrates dyspnea with talking. Patient’s wife states that he currently smokes 5 cigarettes per day which is less than the 2 packs per day, of non filtered Camels, that he was smoking 6 years ago. Patient states“it is hard to quit but I guess it time”. |
Day 3Day 3: Ambulates to bathroom without dyspnea. Voids without difficulty. Patient able to ambulate in hallway 50 feet with 02 at 4 l/NC with moderate dyspnea; maintains O2 sat at 88%. Eating 25-50 % of meals with frequent rest periods. Social Service Case Manager in to do follow up discharge planning.
|
Day 5Day 5: Discharge note: Discussed readiness for enhanced self-care at the pulmonary rehabilitation facility, including feeding, toileting, and dressing. Patient and family relate their goal is to have Henry at home soon. Mr. Henry, his daughter Betty, and wife Ertha verbalize recognition of the high probability of needing supportive services in the home. Medication and oxygen therapy education given. Discuss plans for medication administration and the need for oxygen at the rehab facility and in a home setting. Family verbalizes their concerns about paying for services at home (housing, meals, medications, oxygen, and home care aide). Discharge instructions completed. Report called to the Pulmonary Rehab Unit. Will transfer patient with a copy of his Medical record. |
Physician and PA
Physician and PA Discharge Note
Henry is a 69-year-old male with Chronic Obstructive Pulmonary Disease (COPD) who presents to the Emergency Room with a three-day history of progressive dyspnea, cough and increased production of clear sputum. He usually coughs up only a scant amount of clear sputum daily and coughing is generally worse after rising in the morning. He denies fever, chills, night sweats, weakness, muscle aches, joint aches and bloody sputum. He treated himself with albuterol but respiratory distress increased despite multiple inhalations. Upon arrival in the ER few breath sounds were heard with auscultation. Henry was so short of breath that he had difficulty walking to the exam table. He could not complete a sentence without a long pause. He was placed on 4 liters of oxygen by nasal cannula and given nebulizer treatments. He was then admitted to the hospital for further treatment.
PMH
Hypertension for ten years
COPD diagnosed six years ago
Asthma
Occasional episodes of acute bronchitis treated as an outpatient with antibiotics
History of exposure to TB exposure
Occupational exposure to asbestos
Family History
Father dead of lung carcinoma
Mother died at age 60 from COPD
One sister, developed heart disease in her 50s
Only son deceased
Daughter in-law Betty is alive and in good health
Social History
Married to Ertha for 47 years
History of alcohol use but social drinker for past 15 years
Two pack per day Camel smoker for 37 years but has cut back to 5 cigarettes daily since COPD diagnosed; will consider terminating all smoking
ROS
Denies intentional weight loss but has lost 25 pounds in the past 7 years
Denies progressive fatigue, loss of libido, morning headaches or sleeping problems
Denies itching
No tinnitus
No ear pain
No throat pain
No difficulty swallowing
Denies muscle aches, joint pain, bone pain or back pain
No headache or dizziness
Medications
Advair Discus 250 every 12 hours
Albuterol 2 puffs as needed for acute shortness of breath
Crestor 20 mg every night
Lisinopril 10 mg daily
Lopressor 50 mg daily
ASA 81 mg daily
Singulair 10 mg every night
Vital signs
Pulse120, Respirations 35, BP 130/85, T 100.2F, pO2 87%, Weight 165, Height 67 inches
Physical Examination
General
Anxious, moderate distress, alert
Skin
Warm but pale
Negative for cyanosis, nodules, masses, rashes and jaundice
Negative for ecchymoses and petechiae
Normal skin turgor
HEENT
PERLA
EOMs show full range of motion without pain
Sclera anicteric
Conjunctiva normal
Fundi normal
TMs normal
Nares clear but purse with breathing
Oropharynx normal
Teeth yellowed
Mucous membranes moist
Tongue normal
Neck
Full ROM
No cervical lymphadenopathy, no thyromegaly, no masses, no carotid bruits
Chest and Lungs
No supraclavicular lymph nodes
Barrel chest
Use of accessory muscles at rest
Poor diaphragmatic movement bilaterally
Hyperresonant to percussion
Decreased breath sounds throughout
Prolonged expiration with occasional mild expiratory wheezes
No crackles or rhonchi
Heart
Normal rhythm
Normal S1 and S2
Prolonged S3
No murmurs or rubs
Abdomen
Positive for hepatosplenomegaly, fluid wave, diffuse tenderness and distension
No masses, bruits or distended superficial veins
Normal BS
No CVA tenderness
Genitalia and Rectum
Penis, testes and scrotum normal
Prostate slightly enlarged without nodules
No internal rectal masses palpated
Musculoskeletal and Extremities
Cyanotic nail beds
No clubbing
1+ pedal edema to mid-calves
2+ dorsalis pedis and posterior tibial pules bilaterally
No spine tenderness
Full ROM of back
Normal ROM of extremities
Neurological
Alert and oriented
Cranial nerves intact
Reflexes 5/5 upper and lower extremities bilaterally
Tendon reflexes 5/5 upper and lower extremities bilaterally
Strength normal
Sensation normal
Gait steady
Assessment
COPD with respiratory distress and hypoxemia
Rule out pneumonia
Congestive heart failure
Hepatosplenomegaly
Plan
On admission
CBC with differential
CMP
Electrolytes
UA
Follow pO2
Chest X-ray
BNP
COPD diet
Methylprednisolone 60 mg IV
Atrovent
Albuterol
Respiratory therapy consult
Physical therapy consult
Nutrition consult
Social work consult
Pulmonology consult: antibiotics if indicated
Cardiac consult: evaluation and treatment as recommended
On Discharge
VS P 100, R 24, BP 120/85, T 98.6F, pO2 93%
Chest aeration improved
No use of accessory muscles
Patient improved on COPD/asthma meds
Discharge to pulmonary rehabilitation
Day 1Dx: Exacerbation of COPD, hypoxia, dyspnea, and rule out pneumonia. |
Day 5Discharge patient to rehabilitation facility for follow up with self-care and pulmonary rehabilitation. |
Occupational Therapy
Initial Evaluation – Day 2 of admission
S: “Sure…. I feel great… as long as I don’t try to do anything.” Patient
O: History: Patient admitted yesterday with SOB; diagnosed as acute exacerbation of COPD. PMH: COPD, CVD, asthma, HTN, hearing loss and past smoker. He has dentures, wears bifocals, and has hearing aids. Pt. is on O2, 2l per nasal prong; saturation rates generally around 90% at rest.
Occupational Profile: Patient lives in a one-story apartment with his wife, Ertha, who has dementia. Pt. independent PTA, but expressed difficulty attending to his wife, the house, yard, and car. Past work as an engineer in the transit department, retired 3 years ago. Wife is currently at daughter-in-laws house, as she requires supervision for safely and ADLs.
Observation: pt. was sitting up at the side of the bed, attempting to finish his lunch. Speech was halting and patient was SOB in his attempts to answer the therapist’s questions.
Cognition: Patient alert and Ox4. Able to follow multiple step directions.
Functional Mobility: Supplemental O2 at 2L utilized during all activities. Independent bed mobility and modified Independent ambulation in the room with FWW. C/O mild dizziness with transition from sit to stand. Patient required multiple verbal cues to decrease speed of ambulation and proper use of FWW. CGA sit=stand on 3-in-1 commode over the toilet. O2 sats at 80 following treatment; returned to 92% following rest break and instruction to complete pursed lip breathing, (PLB), for 5 min. Required mod verbal cues for completion of PLB.
ADLs: Independent peri-care after toileting. Patient stood at sink with FWW, CGA, for washing hands and face. Patient reports that he is I with all ADLs at home but needs frequent rest breaks.
ROM: Patient exhibited WFL AROM both UEs while seated in bedside chair.
Strength: formal MMT NT due to SOB. UE strength appears WFL but limited by poor general endurance and SOB.
Role Change Assessment (RCA): Loss in areas such as his church participation, reductions in volunteer activities, decline in previous leisure such as woodworking, and couples bridge. Inability to maintain house; states he has been cited by the HOA 2x in the past year for failure to keep the weeds pulled.
Pain: 0/10 pain on the VAS at beginning of evaluation and at end of evaluation
A: Problem list:
- Poor endurance for ADLs
- Decreased functional mobility
- Decreased knowledge of breathing techniques such as PLB and A-D breathing.
- Loss of roles secondary to declining health and increased caregiver demands at home
- Decreased knowledge of energy conservation techniques
Patient has diminished endurance and functional mobility due to exacerbation of COPD that hinders his ability to complete ADLs. He would benefit from skilled OT for ADL retraining combined with breathing and energy conservation training which would allow for improved ADLs functioning and resumption of caregiver role after discharge.
Goals:
- Patient will exhibit independent use of PLB technique during ambulation in the room in 1 week.
- Modified Independence for toilet transfer in 1 week.
- Modified Independent for showering using a shower seat in 1 week.
- Patient will teach back 4 energy conservation techniques he will use for his morning ADL routine in 1 week.
Plan:
Patient will be seen for occupational therapy services 1x/day for 1 week or until discharge from acute inpatient setting.
Anticipated OT Treatments: ADL retraining, functional mobility, energy conservation and breathing techniques, HEP development. Recommendations for appropriate bathroom equipment. Assist with discharge planning.
Tania Shearon, MOT, OTR/L, CHT 9/22/2017
Treatment note: Day 3 of admission
S: “I really need to get my strength back so I can take care of my wife”.
O: O2 sat is 95% at rest. Supplemental O2 at 2L utilized during all activities including showering. No c/o pain.
CGA assist with FWW to ambulate to bathroom. Educated on use of PLB during ambulation and while seated on toilet; 95% sat after short rest. CGA and instruction on safe technique for stepping backward into showering using FWW. CGA to sit on shower seat. Set up for adjusting water and use of hand-held shower. Patient able to wash upper and lower body with assist for washing his back. Instructed that water should be warm and not hot as this will decrease fatigue during showering task. Patient I drying off and donning clean gown. CGA stepping out of the shower with FWW and ambulation to bedside chair. Sats at 90% following showering activity.
A: Recommend shower seat for home. Patient exhibited improved ability to complete PLB that allowed him to complete showering activity without SOB. Improved understanding of energy conservation techniques and how he can use them at home to improve his functional ability.
P: Continue as per POC.
Tania Shearon, MOT, OTR/L, CHT 9/23/2017
Discharge Summary – Day 5 of admission
S: “I feel stronger and better able to go home and take care of my wife”.
O: Patient has been seen 1x/daily during this admission. D/C planned for this date to a pulmonary rehabilitation center. No c/o pain.
Re-evaluation: Patient able to tolerate MMT screening of both UEs in sitting. 4/5 muscle grade throughout both UEs and hands; 90% sat following MMT screen.
Patient education: Patient able to demonstrate appropriate technique for PLB and A-D breathing while sitting and during ambulation with FWW in room.
Functional mobility: Patient Modified I in the room for ambulation with FWW to toilet and sink. This date, CGA for stepping in and out of shower; continued to requiring verbal cues for safe technique. Sats at 90% during ambulation with FWW utilizing PLB as needed.
ADLs: Modified I standing at sink with FWW for grooming and hygiene. Patient tolerated standing for 7 min. using 02 at 2L.
A: Patient has made good progress toward goals, however, continues to have decreased endurance for functional mobility and ADLs. Pt. has gained ability to self-monitor his own 02 sats and modify the pace of activity and rest periods that will allow him to continue to increase activity levels. Pt. able to tolerate increased ambulation and standing for ADLs in the room with use of energy conservation and breathing exercises
Recommend continued OT at pulmonary rehabilitation unit for ADL training and progression toward IADL retraining. He will need further recommendations for adaptive equipment for home such as grab bars and shower seat. Recommend home health evaluation after d/c from rehabilitation facility to ensure safety and max I with all ADL/IADLs at home.
Goals:
Progress toward goals:
- Patient will exhibit independent use of PLB technique during ambulation in the room in 1 week - Achieved
- Modified Independence for toilet transfer in 1 week - Achieved
- Modified Independent for showering using a shower seat in 1 week – Partially achieved
- Patient will teach back 4 energy conservation techniques he will use for his morning ADL routine in 1 week – Partially achieved
P: Patient to be D/Cd to pulmonary rehabilitation facility to maximize level of functional mobility, safety/independence with ADLs, IADLs and caregiver responsibilities.
Tania Shearon, MOT, OTR/L, CHT 9/25/2017
Physical Therapy
Initial Evaluation - Day 2 of admission
S: ”I’m so tired. I just want to sleep all day.”
O: History: Pt. admitted yesterday with difficulty breathing due to acute exacerbation of COPD. History of COPD, CVD, asthma, HTN, hearing loss (uses hearing aids), and past smoker. Social: Lives with wife in single-level apartment. Wife with history of dementia and is being cared for by daughter-in-law while patient is in hospital. Daughter-in-law (patient’s son deceased) and grandson live a couple of hours from patient. Retired engineer from Transit Department. Patient has been active and independent and expresses interest in travelling and spending time with his family. Precautions: Standard Examination findings:
Observation: Patient lying semi-reclined in bed, 2 liter O2 nasal cannula, IV.
Cognition/language: Alert, oriented to time, place and person. Consistently follows instructions.
Sensation: Light touch and kinesthesia intact bilateral LEs.
Motor: AROM WNL.
Tone: WNL.
Strength: 4/5 hip flexors and knee extensors; 4-/5 hip abductors; 4/5 ankle dorsiflexors and plantarflexors. Balance: Independent sitting. Modified Clinical Test for Sensory Interaction in Balance (CTSIB): Able to maintain standing eyes open and eyes closed on firm surface 30 secs without increased sway; able to maintain standing eyes open 30 secs on foam without increased sway; mild to moderate increased sway standing on foam eyes closed 10 secs. Functional Reach Test: 10 inches. Stands on
one leg eyes open R LE 10.5 secs, L LE 10.8 secs. Stand on one leg eyes closed for 1 sec bilaterally.
Mobility: Independent bed mobility. Modified independent transfers moving between bed and bedside chair. Patient complained of mild dizziness when going from sit to stand, but this resolved quickly. Minimal assistance for walking to bathroom. Able to tolerate sitting for 30 minutes before requesting to go back to bed. Ambulation with 2 liters supplemental oxygen 100’ level surfaces with minimal assistance, stopping 1 time momentarily to rest due to SOB. No loss of balance during walking. Slow gait speed. 02 sats at 90% prior to ambulation, 88% immediately after ambulation, and then 90% after 5 minutes of rest at end of session, all on supplemental 02. Stairclimbing/steps not assessed. Timed 10-Meter Walk Test using FWW at a comfortable gait speed was 0.5 m/s.
A: Major impairments and activity limitations include:
- LE weakness.
- Limited endurance.
- Possible orthostatic hypotension.
- Impaired single-leg stance balance; impaired ability to use vestibular information for balance.
- Reduced gait speed.
- Minimal assistance for walking indoors on level surfaces.
Goals:
- Increase strength LEs ½ grade for increased use in ADLs.
- No c/o of dizziness with sit to standing.
- Maintain standing on foam eyes closed for 20 seconds to increase ability to use vestibular information for balance.
- Maintain single leg standing balance with eyes open for 20 seconds to improve ability to perform activities such as stair climbing.
- Tolerate sitting up in beside chair at least 1 hour without supplemental 02 and 02 sats above 90%.
- Modified independence walking to bathroom with assistive device.
- Ambulation with assistive device 150’ level surfaces without supplemental 02, without rest periods, with 02 sats above 90% with supervision.
Plan: Therapeutic exercise and mobility training 1-2x/day. Monitor vital signs. Progress sitting tolerance and distance walked. Patient and family education. Discharge planning. Order needed equipment.
Discharge Summary - Day 5 of admission
S: “I feel stronger, but know I need more therapy so I can get back home with my family.”
O: Patient has been seen 1-2x/daily during this admission. He is being D/Cd today to a rehabilitation for continued therapies.
Examination findings:
Cognition/language: Alert, oriented to time, place and person. Consistently follows instructions.
Sensation: Light touch and kinesthesia intact LEs.
Motor: AROM WNL.
Tone: WNL.
Strength: 4+/5 hip flexors; 4/5 knee extensors; 4-/5 hip abductors; 4+/5 ankle dorsiflexors and plantarflexors. Balance: Modified Clinical Test for Sensory Interaction in Balance (CTSIB): Able to maintain standing eyes open and eyes closed on firm surface 30 secs without increased sway; able to maintain standing eyes open 30 secs on foam without increased sway; mild increased sway standing on foam eyes closed 15 secs. Stands on one leg eyes open R LE 18 secs, L LE 17 secs. Stand on one leg eyes closed for 1 sec bilaterally.
Mobility: Modified independent transfers moving between bed and bedside chair. Patient has been instructed to perform several ankle pumps prior to standing from sitting and to come to standing slower and he shows follow through with these recommendations independently. After day 3 of admission, had no complaints of dizziness with sit to stand. Modified independence for walking to bathroom with a front-wheeled walker (FWW). Patient is able to walk short distances without the FWW with supervision, but he feels more secure using a FWW at this time. Able to tolerate sitting for 60 minutes without supplemental 02 before requesting to go back to bed. Ambulation without supplemental oxygen 150’ with a FWW on level surfaces with supervision and no rest breaks. 02 sats above 90% prior to and following ambulation. Slow gait speed continues – comfortable gait speed on 10-meter walk test is 1.1 m/sec. Able to ascend and descending a 8” step with the FWW with minimal assistance.
A: Patient made progress toward goals during this admission. Continues to have impairments of LE weakness, limited endurance, and impaired motor and sensory strategies for balance. Has activity limitations and a need for assistive device for walking and reduced gait speed. Needs continued therapy to progress toward goal of independent and safe mobility. Patient has been educated in safety precautions regarding decreasing episodes of orthostatic hypotension and how to walk safely indoors with the FWW. As he becomes more mobile, he will need to experience walking in a variety of environmental conditions and his need for assistive devices will need ongoing assessment. He needs continued balance assessment and intervention. He will need a home environmental assessment prior to D/C from the rehabilitation facility to ensure independence and safety in the home. Patient’s wife has observed patient in therapy but is unable to assist Henry with mobility due to her cognitive impairment. Patient needs to progress to the level of at least modified independence with all mobility in order to return to home. Patient has potential to progress to this level with intensive in-patient rehabilitation and will need to engage in life-long fitness activities as tolerated.
Goals: Progress toward goals:
- Increase strength LEs ½ grade for increased use in ADLs. – Partially achieved.
- No c/o of dizziness with sit to standing – Achieved.
- Maintain standing on foam eyes closed for 20 seconds to increase ability to use vestibular information for balance. – Partially achieved.
- Maintain single leg standing balance with eyes open for 20 seconds to improve ability to perform activities such as stair climbing. – Partially achieved.
- Tolerate sitting up in beside chair at least 1 hour without supplemental 02 and 02 sats above 90%. – Achieved.
- Modified independence walking to bathroom with assistive device. – Achieved.
- Ambulation with assistive device 150’ level surfaces without supplemental 02, without rest periods, with 02 sats above 90% with supervision. – Achieved.
Plan: Patient to be D/Cd to rehabilitation facility to maximize level of functional mobility and prepare for D/C to home.
Health Educator
Health Education: Community/Public Health:
Profession Description :
Health Education: Community/Public Health:
Profession Description :
The U.S. Department of Labor Bureau of Labor Statistics (BLS) defines health educators (SOC 21-1091.00) as those who promote, maintain, and improve individual and community health by assisting individuals and communities to adopt healthy behaviors, collect and analyze data to identify community needs prior to planning, implementing, monitoring, and evaluating programs designed to encourage healthy lifestyles, policies and environments. They may also serve as a resource to assist individuals, other professionals, or the community, and may administer fiscal resources for health education https://www.bls.gov/oes/current/oes211091.htm
Health educators work to encourage healthy lifestyles and wellness through educating individuals and communities about behaviors that promote healthy living and prevent diseases and other health problems.
Responsibilities and Competencies for Health Education Specialists: http://www.nchec.org/credentialing/responsibilities/
Seven Areas of Responsibility:
Area I: Assess Needs, Resources and Capacity for Health Education/Promotion
Area II: Plan Health Education/Promotion
Area III: Implement Health Education/Promotion
Area IV: Conduct Evaluation and Research Related to Health Education/Promotion
Area V: Administer and Manage Health Education/Promotion
Area VI: Serve as a Health Education/Promotion Resource Person
Area VII. Communicate, Promote, and Advocate for Health, Health Education/Promotion, and the Profession
Brief: Certified Health Education Specialists/Roles and Responsibilities: http://www.sophe.org/healthedspecialist.cfm
Brief Videos: What is Public Health/This is Public Health:
https://www.youtube.com/watch?v=ErBECLCWNOk
https://www.youtube.com/watch?v=oy1CAMObRzc
HEALTH EDUCATION SPECIALIST “CONSULT” – HOSPITAL NOTES AND ASSESSMENTS
Seven Areas of Responsibility: Certified Health Education Specialist
Area I: Assess Needs, Resources and Capacity for Health Education/Promotion
Area II: Plan Health Education/Promotion
Area III: Implement Health Education/Promotion
Area IV: Conduct Evaluation and Research Related to Health Education/Promotion
Area V: Administer and Manage Health Education/Promotion
Area VI: Serve as a Health Education/Promotion Resource Person
Area VII. Communicate, Promote, and Advocate for Health, Health Education/Promotion, and the Profession
Certified Health Education Specialist (CHES) “Consult” - Health Education/Community and Public Health:
“As a health care professional, you assess patients all the time. But you generally do not assess a patient’s family caregiver, except to identify that person as a “resource” or “informal support” when developing a discharge plan. In this traditional view, the family caregiver, who is not a client or a beneficiary and not an official part of the health care team, is typically outside the realm of professional responsibility. Like so much of health care today, that view is changing. Increasingly professionals “hand off” very sick or disabled patients to family caregivers after a hospital stay, a short-term nursing home stay, or an episode of home care services. In these transitions, especially when the patient is elderly or chronically ill, the patients’ continued health and well-being depends on a family caregiver. That person must be willing and able to handle the patient’s complex health, financial, legal, and social needs. Sometimes these tasks are temporary, while the patient recovers; in the case of elderly or seriously ill patients, the job can continue for months or years.
Caregiver assessment is a tool to help identify strengths and limitations to help develop a realistic plan for the next stage of care. The goal is twofold: (1) to ensure that the patient’s health and well-being are maintained and enhanced; and (2) to ensure that the caregiver’s capacities and needs are considered and addressed in a care plan.”
Health Educators conduct “assessments”; so….
“I would recommend…” …A Caregiver’s Assessment: ask Betty about…
• The caregiver’s background, including age, education, employment, other family responsibilities, living arrangements.
• The caregiver’s perception of the care recipient’s health and functional status.
• Length of time the caregiver has been providing care; if is a new event, what the caregiver worries most about in providing care.
• Values and preferences about caregiving (“do it all myself,”; “can’t deal with needles or incontinence,”; “I can’t take Mom to my home because there just isn’t room for another person”).
• Caregiver’s health status, including any limitations relevant to caregiving.
• Impact of caregiving on emotional status, finances, other family members.
• Knowledge, skills, and abilities to perform necessary caregiving tasks.
• Resources used or interested in accessing.
In introducing the assessment process to the family caregiver, the assessor should clarify the goals of the assessment and make it clear that all information (unless specified by the caregiver) will be shared with the health care team in order to develop a care plan. The assessor should also summarize the conversation, so that the family caregiver feels that his or her concerns have been heard. The assessor can emphasize the positives first, and then list the areas where some questions have been raised, and suggest a process for following up. http://www.rosalynncarter.org/UserFiles/Michigan%20Assessment%20Grid.pdf
· Or see if Betty, because she is a nurse, would wish to use: the Caregiver Self-Assessment http://www.caregiverslibrary.org/Portals/0/CaringforYourself_CaregiverSelfAssessmentQuestionaire.pdf
HEALTH EDUCATION SPECIALIST – TRANSITION TO REHAB NOTES AND RESOURCES
“Health Educators plan and implement evidence-based programs/interventions, so I would recommend some resources….”
Patient Education/COPD: https://www.cdc.gov/copd/index.html ; https://www.cdc.gov/copd/resources.html
Public Health Management of COPD: https://www.cdc.gov/copd/pdfs/framework_for_copd_prevention.pdf
Once COPD has been diagnosed, goals of treatment and management include relieving symptoms; preventing and treating disease progression, complications, and exacerbations; improving exercise tolerance, daily activity, and health status; monitoring nutritional needs; and reducing premature mortality. Management should include smoking cessation and abstinence; limiting exposure to secondhand smoke, dusts, fumes, and gases; pharmacological treatment with bronchodilators and corticosteroids; supplemental oxygen therapy; pulmonary rehabilitation; collaborative self-management; and surgery. Clearly, efforts toward patient and professional education should continue to focus on promoting treatment modalities for persons with COPD as well as persons at risk for COPD.
The research/evidence behind community-based exercise/nutrition interventions for chronic disease: http://academiccommons.columbia.edu/catalog/ac:156754
We recommend the Community Guide as a starting point to finding best-practice interventions for nutrition/exercise programs in your community: https://www.thecommunityguide.org/
In Missouri: MICA: http://health.mo.gov/data/mica/MICA/; http://health.mo.gov/data/InterventionMICA/index.html
Patient Education/Resources:
https://www.americannursetoday.com/when-breathing-is-a-burden-how-to-help-patients-with-copd-2/
https://www.thoracic.org/patients/patient-resources/resources/copd-today.pdf
Speech and Language
SPEECH & LANGUAGE PATHOLOGY
Day 2 of Hospital admission
S: Order received from physician for SLP eval and treat as indicated.
O: Oral-motor and bedside swallowing assessment completed.
A: Structures are WNL for ROM, strength, tone, and coordination for speech and swallowing. Due to COPD respiratory status is poor for efficient speech production and safe and adequate swallowing.
P: Return to eval. Pt.’s cognitive status to determine ability to learn strategies to use breath support more efficiently for speech and follow thru with dietary recommendations for safe swallow in order to maintain safe swallow and nutritional needs.
Day 3 of Hospital admission
S: Pt. in bed demonstrating labored breathing. During brief interview Pt. reported he had some difficulty eating due to increased fatigue during mealtime. He also indicated concerns regarding meal time and caring for his wife who reportedly demonstrates an Alzheimer’s dementia and can no longer cook and “does not eat well”.
O: Completed brief cognitive/memory assessment utilizing the St. Louis University Mental Status Examination (SLUMS). Reviewed strategies for breath support while speaking by producing no more than 4 syllables on one exhalation. Discussed trial texture change to a soft diet is indicated with Pt. agreeing to recommendations.
A: Scores on the SLUMS indicated cognitive and memory performance WNL to learn strategies for efficient breath support for speech and swallowing. Pt. demonstrated ability to produce speech as instructed. Pt. at risk for decline in nutritional status due to poor respiratory support while swallowing.
P: Return to assess Pt.’s ability to follow thru with recommendations for speech and swallowing. Discuss concerns about nutritional status with physician, nursing and dietary.
Day 4 of Hospital admission
S: Noted in medical chart physician’s order for soft diet texture and referral to dietary. Nursing noted the Pt. is eating < 50% of his meals.
O: Reviewed SLP recommendations for speaking and swallowing with Pt. reporting he had forgotten until he saw SLP on this visit. Pt. repeated10 sentences imitating 4 syllable phrase production as demonstrated by therapist. Provided 10 additional sentences requesting Pt. to produce with adjusted phrase production (100%). Discussed dietary concerns indicated by nursing.
A: Pt. understands recommendations for speech and swallowing, but is having difficulty with follow thru. As his cognitive status appears to be WNL for tasks, emotional state may be the issue.
P: Discuss emotional status with social work. Provide Pt. with written instruction of SLP recommendations for DC to rehab.
Day 5 of Hospital admission
S: Pt. preparing for DC with nursing assist as therapist entered room.
O: Provided Pt. with written instructions for 4 syllable speech production on each breath. Encouraged Pt. to share these instructions with rehab SLP. Recommended to Pt. that he discuss with SLP and other rehab staff how he can best meet his dietary needs and assist his wife in meeting her dietary needs and address issues with her memory loss.
A: Pt. appeared to understand instructions and agreed to address them in rehab. but may require reminders from case manager.
P: Provide copy of written instructions and recommendations for SLP to DC planner.
Dental
S: Henry is a 69 yo man with COPD who presents to the ED with a three day history of progressive dyspnea and cough
CC: “Loose denture and burning mouth”
Med HX:
COPD diagnosed 6 years ago.
Occasional episodes of acute bronchitis treated as outpatient with antibiotics.
History of TB, asbestos exposure, occupational exposure, asthma
He denies fever, chills, night sweats, weakness, muscle aches, joint aches and blood in the sputum. He treated himself with albuterol, but respiratory distress increased despite multiple inhalations. Patient was so short of breath that he had difficulty climbing up onto the examiner’s table and completing a sentence without a long pause. He is placed on 2L oxygen via nasal cannula and given nebulizer treatments.
Allergies: NKDA
Med HX:
Advair Discus 250 every 12 hours
Albuterol 2 puffs as needed for acute shortness of breath
Crestor 20 mg every night
Lisinopril 10 mg daily
Lopressor 50 mg daily
ASA 81 mg daily
Singulair 10 mg every night
Social Hx: Married to Ertha
2 pack/day Camel smoker for 37 years has cut back to 5 cigarettes/day since he was diagnosed with COPD and is now willing to consider complete smoking cessation.
Alcohol use, a social drinker for the past 15 years
Denies weight loss but has lost 25 pounds in the last 7 years.
Dental Hx:
Pt has dental phobia. According to him this is the reason he lost most of his teeth. MX. Upper denture is only 4 years old but it is loose now. Pt reports that denture and partial denture do not fit well. Pt is satisfied with the look of his teeth. Pt has trouble chewing food bc denture “clicks” or comes loose while chewing. Pt reports slight sensitivity in lower L posterior occasionally, no pain. Pt doesn’t remember having a dental cleaning.
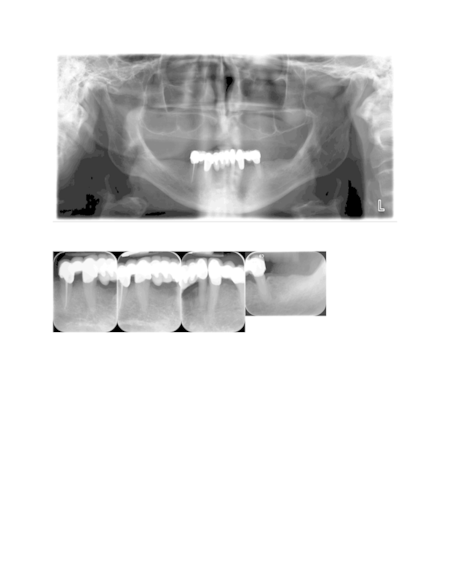
O:
BP: 133/91 mmHg P: 69 bpm
Blood sugar: 145 mg/dL
Clinical Exam:
EOE: raised, firm nodule on L temopral region near hairline 10mmx6mm, L forehead 1/2 inch x 1/2 inch scar from hx of basal cell carcinoma
IOE: Bilateral bone depression between ridge and RMP. Redness under denture along with some white patches. Redness around the corner of the mouth.
TMJ: R pop upon opening
OSC: Negative
Hard Tissue: Pt has full upper denture
Lower has FPD on lower with 29, 27, 23, 22, & 20 as retainer teeth
20: recession, check after SRP
22: check after SRP
23: check after SRP
27: recession, check after SRP
29: check after SRP
Teeth seem sound, but recheck margins of crowns after cleaning
A:
Candidiasis / Angular cheilitis
Perio Dx: Generalized chronic periodontitis
Perio Risk: moderate due to long-span bridge forces
Caries risk: high due to dry mouth
OC risk: high due to smoking
Athletic Training
Athletic Training competencies
AC-2: Differentiate the roles and responsibilities of the athletic trainer from other pre-hospital care and hospital-based providers, including emergency medical technicians/paramedics, nurses, physician assistants, and physicians.
AC-6: When appropriate, obtain and monitor signs of basic body functions including pulse, blood pressure, respiration, pulse oximetry, pain, and core temperature. Relate changes in vital signs to the patient’s status.
AC-7: Differentiate between normal and abnormal physical findings (eg, pulse, blood pressure, heart and lung sounds, oxygen saturation, pain, core temperature) and the associated pathophysiology.
AC-16: Explain the indications, application, and treatment parameters for supplemental oxygen administration for emergency situations.
AC-17: Administer supplemental oxygen with adjuncts (eg, non-rebreather mask, nasal cannula).
AC-32: Determine when use of a metered-dosed inhaler is warranted based on a patient’s condition.
AC-33: Instruct a patient in the use of a meter-dosed inhaler in the presence of asthma-related bronchospasm.
AC-43: Instruct the patient in home care and self-treatment plans for acute conditions.
PD-10: Develop healthcare educational programming specific to the target audience (eg, clients/patients, healthcare personnel, administrators, parents, general public).
PHP-3: Identify modifiable/non-modifiable risk factors and mechanisms for injury and illness.
PHP-5: Explain the precautions and risk factors associated with physical activity in persons with common congenital and acquired abnormalities, disabilities, and diseases.
PHP-19: Instruct clients/patients in the basic principles of ergodynamics and their relationship to the prevention of illness and injury.
CE-7: Identify the patient’s participation restrictions (disabilities) and activity limitations (functional limitations) to determine the impact of the condition on the patient’s life.
CE-8: Explain the role and importance of functional outcome measures in clinical practice and patient health-related quality of life.
CE-9: Identify functional and patient-centered quality of life outcome measures appropriate for use in athletic training practice.
CE-20d: functional assessment
CE-20f.4: balance
CE-21a.2: gait
CE-21a.3: movement patterns
CE-21d: Assessment of quantity and quality of osteokinematic joint motion
EBP-12: Describe the types of outcomes measures for clinical practice (patient-based and clinician-based) as well as types of evidence that are gathered through outcomes assessment (patient-oriented evidence versus disease-oriented evidence).
EBP-14: Apply and interpret clinical outcomes to assess patient status, progress, and change using psychometrically sound outcome instruments.
PS-3: Describe how psychosocial considerations affect clinical decision-making related to return to activity or participation (eg, motivation, confidence).
CE-20g.4: peak-flow
CIP-8: Demonstrate the ability to recognize and refer at-risk individuals and individuals with psychosocial disorders and/or mental health emergencies. As a member of the management team, develop an appropriate management plan (including recommendations for patient safety and activity status) that establishes a professional helping relationship with the patient, ensures interactive support and education, and encourages the athletic trainer’s role of informed patient advocate in a manner consistent with current practice guidelines.
HA-22: Develop specific plans of care for common potential emergent conditions (eg, asthma attack, diabetic emergency).
TI-7: Identify patient- and clinician-oriented outcomes measures commonly used to recommend activity level, make return to play decisions, and maximize patient outcomes and progress in the treatment plan.
TI-10: Integrate self-treatment into the intervention when appropriate, including instructing the patient regarding self-treatment plans.
TI-11: Design therapeutic interventions to meet specified treatment goals.
TI-11d: Instruct the patient how to correctly perform rehabilitative exercises.
TI-11e: Apply the intervention, using parameters appropriate to the intended outcome.
TI-17: Analyze gait and select appropriate instruction and correction strategies to facilitate safe progression to functional gait pattern.
TI-18: Explain the relationship between posture, biomechanics, and ergodynamics and the need to address these components in a therapeutic intervention.
TI-27: Describe the common routes used to administer medications and their advantages and disadvantages.
TI-28: Properly assist and/or instruct the patient in the proper use, cleaning, and storage of drugs commonly delivered by metered dose inhalers, nebulizers, insulin pumps, or other parenteral routes as prescribed by the physician.
TI-29: Describe how common pharmacological agents influence pain and healing and their influence on various therapeutic interventions.
TI-30: Explain the general therapeutic strategy, including drug categories used for treatment, desired treatment outcomes, and typical duration of treatment, for the following common diseases and conditions: asthma, diabetes, hypertension, infections, depression, GERD, allergies, pain, inflammation, and the common cold.
TI-3: Optimize therapeutic outcomes by communicating with patients and/or appropriate healthcare professionals regarding compliance issues, drug interactions, adverse drug reactions, and sub-optimal therapy.
Athletic Training Treatment/Contribution
Ergonomics: Walking, rising from chair, sitting, stepping up and over, reaching
Activities of daily living: gardening at local plots, grooming
High Blood pressure: aerobic activities to reduce BP (stationary bike, walking, walking trails, treadmill)
COPD: demonstrate appropriate use of inhaler, possibly add spacer, teach how to use oxygen
Breathing treatments: sing song/repeat phrase for lung strengthening, demonstrate how to monitor on home spirometer (testing lung capacity)
Provide medication education
Strengthening: low weights/high reps, machine usage at gym or rehab facility, pool workouts – maintain strength gains, explain importance for quality of life
Balance exercises single and double leg, posture
Range of motion exercises for ADLs (dressing)
How to monitor improvements
Provide at home exercises
Explain why important for quality of life
Both can do these exercises
Organize medications
Nutrition education
Social Work
Social Work Clinical Note
S/O Pt. is a 69 year old African-American male being referred to social services for assistance with determining discharge plans. Pt. was admitted four days ago for treatment related to COPD. He was so out of breath at the time of admission that walking to the exam table presented as a challenge. The patient reports having a wife of 47 years. He reports that his wife experiences health problems of her own related to her memory. These problems impact her ability to perform daily tasks such as cooking, self-care, and taking medications the way they are prescribed. The patient goes on to say that his wife gets confused and is very forgetful. He states that all of this contributes to a significant amount of anxiety for him as he must supervise all of her activities. When presented with options for discharge, the patient states that he wants to continue living with his wife.
A The patient appears to be experiencing a decline in his ability to perform self-care. Further, he appears to be in a caregiver role for his wife, and that his wife is not an appropriate source of support. Independent living will not be a suitable situation long-term. The patient will need assistance with basic self-care including but not limited to meal preparation, transportation, medication monitoring, and potentially bathing. Based on patient report, his wife appears to need a similar level of care.
P 1. Information and referral for assisted living facilities.
2. Information and referral for home delivered meals.
3. Information and referral for transportation assistance.
Submitted by:
Charlotte Hansen, MSW
