 The largest military hospital outside the continental US, it is run by the US Army and the Department of Defense. It receives soldiers from Iraq and Afghanistan, as well as military personnel stationed in Germany and their families, and ocassionally civilians. With over 500 beds, it also has all surgical subspecialties and every allied health profession, including OT, PT, speech therapy and dental care.
The largest military hospital outside the continental US, it is run by the US Army and the Department of Defense. It receives soldiers from Iraq and Afghanistan, as well as military personnel stationed in Germany and their families, and ocassionally civilians. With over 500 beds, it also has all surgical subspecialties and every allied health profession, including OT, PT, speech therapy and dental care.
Case Notes
Audiology
Audiology Assessment
Landstuhl Regional Medical Center, Germany
1. Pre-operative audiometrics:
a. Complete audio to determine type and severity of hearing loss considering the damage to the pinna and tympanic membrane, possible acoustic trauma and temporal bone fracture.
2. Post-operative audiometrics:
a. Repeat complete audio to assess type and severity post pinna and tympanic membrane reconstruction.
Diagnosis
1. Pre-operative diagnosis: severe mixed hearing loss in the left ear and normal hearing sensitivity in the right ear.
2. Post-operative diagnosis: pre-op conductive component resolved due to surgical intervention. Mild to severe sensorineural hearing loss across frequencies 250-8000 Hz remains from acoustic trauma.
Plan
1. Monitor post-op care of pinna and tympanic membrane.
2. Repeat audiometric evaluation monthly to monitor thresholds in the left ear for possible recovery of the sensorineural hearing loss.
Medical and Physician Assistant
Admission Medical H&P
Landstuhl Regional Medical Center, Germany
Date: 4-21-2011
HPI : Patient presented to trauma bay with multiple blast injuries. Was embedded with local unit, on patrol in Humvee when IED (improvised explosive device) exploded near left front tire. Patient sustained blast injuries to left face and ear, left shoulder, left chest, left flank, and LLE (left lower extremity).
PMH: Medical records not initially available, patient unable to give detailed history prior to intubation.
Medications: none known
Allergies: NKDA (no known drug allergies)
Immunizations: Last Td (Tetanus-diptheria)> 5 years ago
Past Surgical hx: Appendectomy age 12, SCC (squamous cell carcinoma) removed left cheek mole 2002, no sequellae.
Family Hx: unobtainable
Social Hx: Married, denies tobacco or illicit drug use, occasional ETOH (alcohol)
Religion: agnostic
PE:
Mental Status: Somulent. Difficult to assess because of status and intubation.
Vitals Signs: Initially: Pulse 120, Respiration 24 labored, BP 90/75, Temp 99, Pulse oximetry: 91% on room air, 92% after intubation with FiO2=100%. After 2 liters RL: Pulse 106, Respiration 12 by vent, BP (blood pressure) 116/78.
HEENT: Contusions, superficial lacerations, and abrasions noted along the entire left side of his face and neck. Scant blood is seen in left external auditory meatus. No TM (tympanic membrane) is seen on the left; intact TM is seen and pearly gray on the right. No fluid from the right ear. No palpable skull defect; shrapnel in left temporal/parietal scalp/skin, but no obvious puncture into skull appreciated on initial palpation. No periorbital edema or bruising or bruising over the mastoids. PERRL (pupils equally round and reactive to light) at 4 mm each. Conjunctiva non-injected. Trachea midline without shift; thyroid without noted enlargement or nodularity; carotid upstrokes normal bilaterally without bruits, mandible swollen with some broken teeth noted. Oral exam incomplete because of intubation. Tongue midline and dry. Cranial Nerves 2-12 reported grossly intact prior to intubation. CN 8 is incompletely assessed at this time as is CN 1. Cervical collar in place.
Chest: Lung sounds reveal crackles bilaterally, no tracheal shift. Symmetric chest movement but labored breathing prior to intubation. Minor lacerations and abrasions noted on the left chest wall. Left axillary adenopathy appreciated.
Cardiac: Tachycardic, no murmurs, no gallops. No muffling of heart sounds. No palpable thrills; PMI at left 5th left intercostal space
Abdomen: Multiple abrasions, contusions, and lacerations over left flank and left lower quadrant. Several minor abrasions and superficial lacerations over anterior left upper quadrant. Tender on left abdomen from abrasions; no rebound, no guarding—otherwise soft and non-distended.
Back: Patient is “log-rolled” holding c-spine in place; except for abrasions and contusions on the left-side/left flank (about 10% BSA-Body Surface Area), no obvious injury, malformation, or deformity of the back.
GU: Normal adult male; circumcised, testes palpable without masses; no blood at urethral meatus. Rectal exam reveals normal sphincter tone and is hemoccult negative, prostate 2+, symmetric, no nodules
LUE: No fractures, full PROM (passive range of motion), equal pulses, no edema. Moving spontaneously. Numerous abrasions over scapular area.
RUE: No fractures, full PROM, intact equal pulses, no edema. Spontaneous movement.
LLE: Open fracture of the mid-shaft of the femur. Distal pulses intact, symmetric at 2+/2+. DP/PT (dorsalis pedis/posterior tibialis) pulses bilaterally equal. Wound over open fracture site has some dirt and abrasions. About 1 cm of femur is extending through skin. Unable to flex left knee on presentation; concern for fracture of patella. Left inguinal adenopathy appreciated. Plantar reflex down-going.
RLE: No fractures, full PROM, intact equal pulses, no edema. Decreased spontaneous movement. Plantar reflex down-going.
Impression: Penetrating trauma, blunt force trauma, possible Closed Head Injury (CHI), tachypnea, tachycardia, mild hypotension from blood loss, left TM rupture, left pinna tear/laceration, multiple contusions and minor lacerations/abrasions of left flank, left leg, left shoulder and left chest and abdomen; contaminated, open femur fracture of left leg.
Plan:
1. Continue ventilator support until post-operative period.
2. Maintain coma with pentobarbital
3. CT Head, neck, chest, abdomen
4. Cefepime 2gm IV q12hrs
5. Maintain left leg immobilization with traction splint pending surgical repair; monitor pulse frequently
6. Continue cervical spine precautions until neck is cleared with CT of neck
7. Cardiac monitoring, pulse oximetry
8. Foley catheter care. Monitor I and O
9. CBC and differential, Comprehensive/complete Metabolic Profile, arterial blood gas, UA, Type and Cross 2 units packed red blood cells (prbc), PT/PTT
10. IV NS at150 cc/hour.
11. NG (nasogastric) tube to intermittent suction
12. Wound care bid
13. Fentanyl iv
14. Pneumatic compression device right LE
15. Neurosurgical consult
16. Orthopedic consult
17. Dental consult
Osteopathic
Admission Osteopathic Palpatory Evaluation
Landstuhl Regional Medical Center, Germany
This additional information was obtained after the initial medical history and physical and after the patient was transferred, stabilized, and while awaiting surgical intervention and cervical spine clearance. Limited evaluation. Noted slight edema formation about areas of wounds.
Head:
Noted left facial and head trauma-open wounds, lacerations, and abrasions. Left occipital condylar compression. Limited evaluation due to coma and ventilator.
Cervical: restricted examination due to cervical collar and intubation.
Thorax: elevated left clavicle; inhalation restriction ribs 1-4 on the left; exhalation somatic dysfunction of the thoraco-abdominal diaphragm with restriction of ribs 6-8 on the right, 8-12 on the left, and inhalation somatic dysfunction ribs 10-12 on the right; nodularity left 3 and 4 ics anteriorly; increased paravertebral muscle tone T1-6 bilaterally and T8-12 left greater than right.
Lumbar: limited evaluation-increased paravertebral muscle tone in the thoraco-lumbar and overall lumbar region bilaterally; lumbo-sacral compression
Abdomen: noted abrasions, lacerations, and contusions on the left flank and side.
Sacrum: limited evaluation-sacral torsion
Pelvis: limited evaluation-posterior left innominate; positive left SI compression test; restricted pelvic diaphragm
Upper Extremities: limited evaluation-no fractures noted. Some abrasions on the left. Intravenous access bilaterally.
Lower Extremities: open left femoral fracture. Examination limited
Impression: Additionally see medical admission H and P for this facility
1. Multiple somatic dysfunctions of the head, cervical/thoracic/lumbar/ sacral spines, pelvis, abdomen, upper and lower extremities.
2. S/p head injury with temporal fracture on ventilator in a medically induced coma
3. Contaminated, open left femoral fracture
4. Pulmonary contusion left
5. Ruptured left tympanic membrane
6. Broken teeth
Plan:
1. OMM to start after surgical intervention. Dosing dependent upon condition and patient tolerance. Will continue to monitor.
2. Care as per medical and surgical team
Nursing
SBAR Report-Nursing- Germany
Given by: L. Wald, BSN, RN
Date of Report: 5-23-11
Jones, Charles Robert (Chip) MRN: 593231
38 year old Male
Code status: Full Code
Allergies: NKA
Weight: 98kg/ 215lbs Height: 6’ / 72”
Admitting Diagnosis: Trauma
Brief History of hospital course: Riding in Humvee on photo shoot with military, struck by improvised explosive device (IED). Sustained serious injuries to left side of body including arm, leg, chest, and head/face.
Family/Social Concerns: Wife, Nancy and 3 children under 10 living in Tubac, Arizona
His parents live in Tucson, and wife’s parents live in Tubac. Patient is a photographer & videographer. Wife arrived 5/19, care team family conference today with wife.
Body SystemNeuro: |
InterventionContinuous monitoring, Q4 hour & prn assessments per protocol. Percocet PO q 4 hrs . Pre-medicating before therapy scheduled, and PRN |
ResponsePt rests quietly with eyes closed. Intermittently follows commands. Pt states pain is at a 3/10 following Percocet. Improvement in tolerance with therapy noted. |
| Respiratory: Upper R/L-clear/rhonchi Lower R/L – crackles/crackles Lung expansion-symmetric Breathing pattern-symmetric Extubated 4/30. O2 4L via NC SaO2: 94% Productive cough Sputum – Moderate, green |
Continuous monitoring, Q4 hour & prn assessments per protocol. Incentive spirometry x 10 per hour, encourage turn/cough & deep breathing Q 2hrs while awake. Titrate O2 to keep sats >92% Continuous monitoring, Q4 hour & prn assessments per protocol. |
SaO2 99% |
| Cardiac: Heart Rhythm: Sinus Tachycardia Heart Rate: 110-120 Cap Refill: <2 seconds Turgor: brisk Radial pulses 3+ bilaterally Femoral pulses 3+ bilaterally Popliteal pulses 2+ bilaterally Dorsalis pedis pulses 2+ bilaterally |
Continuous monitoring, Q4 hour & prn assessments per protocol. |
Vital signs stable. WNL, assessment WNL. |
| GI/GU: Bowel Sounds: Normoactive x 4 Abdomen: Soft, not-tender Urine: Foley D/C’d, Voids, Clear, yellow. Stool: Formed, hemoccult negative NGT D/C’d Diet: Mechanical soft Nine teeth extracted – pt has difficulty eating. |
Continuous monitoring, Q4 hour & prn assessments per protocol. Monitor I & O, U/O, daily weight. Encouraging soft diet & oral fluids. |
Formed stool x 1.
Urine drainage clear, yellow. |
| Integumentary Lips: moist, pink Mouth: moist, pink Color: light pink undertones Texture: Smooth Incisions/wounds: multiple healed abrasions, contusions, lacerations to left side of scalp, face & L ear, LL flank & LLQ, L knee, Open fracture LLE. External fixator in place |
Sterile dressing changes with sodium chloride. Pin care BID. |
Dressing clean, dry and intact. Redness and warmth noted on LLE. |
| Lines: Peripheral: 20G RFA started 6/23, 18G RFA started 6/24 Central Line D/C’d Arterial Line – D/C’d |
No redness, swelling or discharge noted |
| Vitals: T 99.2 HR 86, BP 125/86, RR 16, SaO2 93%. |
VS Q 2 hours & prn per protocol | VS WNL |
Nursing May 23 Family Meeting
Medical Staff and I met with the patient’s wife Nancy after she visited Chip. Nancy is visibly upset and has lots of questions regarding her husband getting back to normal. Explained to Nancy that we can update her regarding Chip’s status at any time. Reassured patient that he is getting the best care possible.
Occupational Therapy
Occupational Therapy Evaluation
Landstuhl Hospital, Germany
Date: 4/26/12
S: 0 (pt is not responding verbally). Pt moans intermittently as he is being repositioned.
O: Orders for OT received. Pt is a 38 yr old male transported to this German hospital from a US military field hospital in Afghanistan. Chart reveals multiple injuries, mainly to L side of body and including a skull fracture due to an assault with an IED. He has had surgical repair of the L skull fracture. He has injuries to the L ear and multiple teeth have been extracted. He has external fixator to L Femur due to multiple FX. He has foley draining light colored urine without cloudiness. Chart reveals vitals are stable. BP elevates while being repositioned in bed. Pt is supine in hospital bed with L leg elevated. According to nursing, he will be kept sedated in order to aide healing and in order to quiet the brain while it is determined the full extent of his injuries. In anticipation of this OT eval, they have backed off on some of the sedation temporarily. Nurses report he is increasingly agitated each time a transport chopper arrives at the helipad. He is not responsive to calling out his name. He does open his eyes briefly when loudly commanded to do so. When loudly asked to squeeze the therapists hand with his L or R hand, he is able to do so, but more weakly on the R side. After this much, pt is again sedated too much to actively participate in the eval. Pt became restless/slightly agitated while being moved, but calmed when the aide who was restocking linens began singing old Beatles songs.
AROM- Pt too sedated to accurately assess
PROM- Pt moans intermittently when R hand is evaluated. Pt has abnormal flexor tone in R hand. Skin is smooth and tight across MCPs. Full passive range of MCPs, PIPs and DIPs cannot be obtained without pain. R hand is edematous. Thumb opposition is impaired by pain/edema.
Strength- Unable to accurately assess. Pt too sedated to participate.
Visual Tracking- Pt can keep his eyes open briefly and gaze to the left but does not sustain gaze as therapist moves to the R side of the bed.
Hearing- TBD Awaiting Audiology report.
PLOF- Pt is an American photojournalist. Married with 3 children. Wife may be on her way to Germany but arrival date unclear at this time.
TX this visit. OTR provided gentle PROM to bilateral UEs including scapular mobilization, Shoulder, elbow, wrists and all digits. OTR encouraged nursing to position both wrists in slight extension and with washcloth rolled in hands to preserve hand mobility. OTR encouraged frequent repositioning.
A: The following will be addressed by OT:
1. MAX A all ADL/ IADL
2. Risk of UE contractures due to immobility
3. Sedation with unknown possible combination of cognitive, hearing, visual impairments
4. Strengths:
Vitals stable
Able to respond to strong verbal stimuli
Stable work hx, Highly educated. Married with 3 children.
P: OT 1-2x day until transfer to the US.
Goals for OT:
1. Increase ability to sustain visual gaze/follow verbal commands x 1 min.
2. Prevent UE contractures with PROM as tolerated. Reduce UE edema with elevation and retrograde massage
3. Obtain more info about meaningful occupations that may be used to promote involvement in treatment and instill hope. Meet with wife as soon as possible in person or by phone.
Speech and Language Pathology
Speech/Language Therapy
Landstuhl Regional Medical Center, Germany
Initial Evaluation – 4/26/11
S: Orders for SLP assessment received. Pt lying in bed and not responding to his name being called. Pt. intubated and IV, foley catheter, and NG tube in place.
O: History: Pt’s chart reviewed. The 38 yo male Pt was a victim of a blast injury due to an exploding IED on 4/19/11 while embedded with the U.S. military in Afghanistan. He is a civilian employed as a photo journalist. He sustained multiple injuries particularly to the left side of his body with obvious head trauma. He arrived in a medically comatose state.
The Pt is married with 3 children. His wife reportedly is arriving in Germany when she can make arragements to do so.
Assessment: The pt was not able to participate in formal assessment due to level of sedation. He inconsistently opened his eyes in response to auditory stimulation (yes/no questions, simple commands, and music). He obviously has some level of comprehension as when he did respond to yes/no questions and simple commands his responses were correct. These responses occurred less than 50% of the time. There were no attempts to vocalize, but the Pt reportedly has become agitated at times according to nursing.
A: The Pt is currently in a state of decreased awareness due to his medical state.
P: Goals will be to assess/monitor daily to identify any improved processing and to increase ability to respond to stimuli (auditory, visual, and/or tactile). Co-treatment with other disciplines will be discussed with these disciplines.
Physical Therapy
Physical Therapy
Landstuhl Regional Medical Center, Germany
Initial evaluation: 4/25/11
S: Pt lying semireclined in bed, external fixator left (L) lower extremity (LE). Intubated, IV, foley catheter, NG tube.
O: History: Pt. admitted 4/21/11 from Afghanistan after sustaining multiple blast injuries from IED on 4/19/11. Injuries include, possible closed head injury (CHI); shrapnel L scalp; L tympanic membrane (TM) rupture; multiple contusions and lacerations/abrasions of L scalp, face, ear, flank, leg, shoulder, chest and abdomen; contaminated, open L mid-shaft comminuted femur fracture; teeth/possible mandible injury. L LE was immobilized in traction splint in Germany. Glasgow Coma Score of 10 initially and patient in medically-induced coma for transport to Germany. External fixator applied to L femur fracture 4/24/11; fracture remains open due to concern of infection.
Social: Married, 3 children, works as a photo journalist.
Precautions: Cervical precautions, cervical collar at all times; multiple abrasions; open femur fracture; Non-weight bearing (NWB) L LE.
Examination findings:
Cognition/language: Eyes closed much of session, lethargic. Opens eyes briefly intermittently during session, particularly in response to movement of extremities and when sitting up at edge of bed and in chair. Follows simple verbal commands inconsistently. Nods yes/no appropriately inconsistently in response to questions. Reportedly was speaking in 1-2 word utterances in Afghanistan prior to intubation.
Sensation: Difficult to test sensation due to decreased level of alertness, but light touch appears intact right (R) upper extremity (UE), R LE, L UE, and distally L LE. Responds to stimuli presented in L visual field more often than when presented in R visual field
Motor: PROM intact R UE (although R hand is edematous and patient grimaces inconsistently with stretching of fingers), R LE, L UE; L LE: Unable to fully assess but hip flexion at least 70 degrees, knee flexion 50 degrees, ankle dorsiflexion 5 degrees.
Strength: Moves R UE, LUE, R LE and L ankle spontaneously and inconsistently to command. Has at least 2/5 strength R UE and LE, 3/5 strength L UE, and 3/5 L ankle dorsiflexion/plantarflexion; at least 1/5 L hip flexion and L knee extension. Grimaces with PROM/AROM of L LE.
Balance: Able to maintain sitting at edge of bed with minimal assistance for @ 5 minutes.
Mobility: Maximum assistance of 2 for moving supine to sitting at edge of bed. Maintains sitting with minimum assistance for @ 5 minutes before fatiguing. Maximum assistance of 2 for sliding board transfer bed to bedside chair, transferring to R. L LE elevated on pillows in chair. BP 115/80 at start of treatment; increased to 135/80 during supine to sit, but returned to 120/80 after sitting @ 5 mins.
A: Major impairments and activity limitations include:
1) Inconsistently following verbal commands
2) Possible R UE and LE weakness
3) Possible R visual field cut
4) L LE limited PROM, strength and pain due to femur fracture
5) Impaired balance in sitting
6) Limited endurance
7) Maximum assistance for all mobility. NWB L LE
Goals:
1) Increase strength R UE and LE and L UE to 4/5 for increased use in ADLs.
2) Increase PROM R hip and knee flexion to 90 degrees flexion.
3) Able to perform simple functional tasks in sitting with supervision.
4) Sliding board transfers to bed, chair, commode with moderate assistance of 1.
5) Tolerate sitting up in wheelchair at least 2 hours.
6) Modified independence manual wheelchair propulsion 300’.
7) Ambulation with FWW 150’ level surfaces with minimal assistance, NWB L LE.
Plan: Therapeutic exercise and mobility training 1-2x/day.
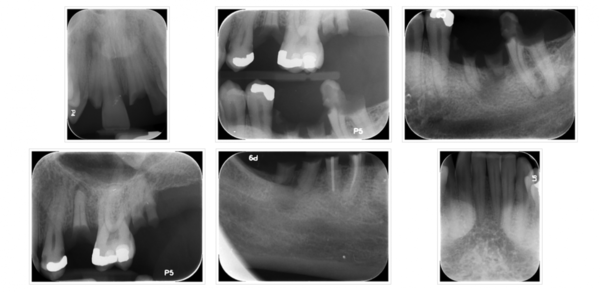
Dental
Dental
Landstuhl Regional Medical Center, Germany
Extraction of fractured teeth / non-restorable:
FDI numbering system
#12, 21, 25, 27, 36, 37, 45, 46, 47
X-Rays Taken Prior to Extraction of Fractured Teeth