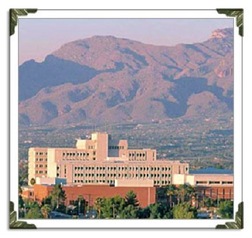
 Located in the heart of Tucson, Arizona, Gila Hospital is a 500-bed, not-for-profit hospital that provides a wide range of health, social and support services. Gila Hospital is a nationally recognized center for quality tertiary care, medical education and research. It is a Level I Trauma Center verified by the American College of Surgeons and is also a respected center for maternity care, orthopedics, oncology and many other medical services. Gila Hospital offers both inpatient and outpatient services.
Located in the heart of Tucson, Arizona, Gila Hospital is a 500-bed, not-for-profit hospital that provides a wide range of health, social and support services. Gila Hospital is a nationally recognized center for quality tertiary care, medical education and research. It is a Level I Trauma Center verified by the American College of Surgeons and is also a respected center for maternity care, orthopedics, oncology and many other medical services. Gila Hospital offers both inpatient and outpatient services.
Inpatient services
Acute care services are delivered at Gila by teams of health care professionals from a range of medical and surgical specialties. Hospital-based acute inpatient care has the goal of discharging patients as soon as they are deemed healthy and stable.
The Gila Medical Group is the employed physician group of Gila Hospital. Gila Medical Group employs more than 250 providers and 200 support staff that cover a wide variety of specialties. The physicians provide clinical services in their areas of specialty and many serve in pivotal research and leadership roles. The Gila Medical Group also has 200 residents and 10 fellows throughout 15 academic residency and fellowship programs. Medical school students also rotate through the Gila Medical Group.
Expert nursing care is provided with appropriate nursing to patient ratios required for safe and effective care. The nursing staff includes highly qualified nurse practitioners, registered nurses and nursing assistants.
Acute care therapy services include Physical Therapy, Speech Language Pathology and Occupational Therapy. These services are provided in the patient’s room immediately following a surgery or an illness. The therapists work with patients at all levels of care from general admission to intensive care units. Therapists use a team approach working with nursing, physicians and other disciplines to get the patients up and moving sooner and decrease their time in the hospital. The acute care therapists liaise with therapists in rehabilitation and skilled nursing units, home health, and outpatient clinics to ensure a smooth transition for patient care across the continuum.
Case Notes
Audiology
Audiology Assessment
Gila Hospital, Inpatient
1. Monthly audiometric monitoring of left ear thresholds.
2. Serial monitoring of hearing thresholds (conventional and high frequency) and otoacoustic emissions for ototoxicity.
3. Tinnitus evaluation due to complaint of tinnitus.
Diagnosis
1. Mild to severe sensorineural hearing loss across frequencies 250-8000 Hz in the left ear (acoustic trauma). No significant change in thresholds in the left ear when compared to prior post-op studies.
2. Normal hearing sensitivity in the right ear. No evidence of ototoxicity bilaterally.
3. Transient non-specific tinnitus.
Plan
1. Patient counseling regarding tinnitus.
2. Hearing aid fitting for the left ear.
Medical and Physician Assistant
Admission Medical H&P
Gila Hospital, Tucson, AZ
Date: 6-25-2011
HPI: Patient presents to Gila Hospital- Tucson, from Landstuhl Regional Medical Center-Germany for treatment following blast injuries sustained 4/19/2011. The patient was embedded with a Marine military unit and was on patrol when an IED exploded near left side of vehicle. Patient sustained blast injuries to left face and ear, left shoulder, left chest, left flank, pulmonary contusion, head injury, and a compound left femur fracture.
He was stabilized in a combat surgical hospital in Afghanistan with intubation, gross wound care, Td immunization, prophylactic antibiotics (Ancef 1 gm.), fracture stabilization, NG tube, IV fluids, Foley catheter. The patient was intubated. A Fentanyl drip was started for pain control. He was additionally placed in a medically induced coma and transferred to Landstuhl Regional Medical Center in Germany on 4/21/11.
Chip was awakened from the coma on April 23rd but remained on the ventilator until April 30th due to the pulmonary contusion and concern for brain edema. Debridement and external fixation of the left femoral fracture occurred on April 24. The wound was left open to heal by secondary intention because of the concern for infection. On April 28th, Chip developed pneumonia and was continued on Cefepime 2 gm ivpb q 12h confirmed by culture sensitivity. This resolved after ten days without further complications. Additionally he developed osteomyelitis at the femoral wound and pin sites and was placed on Rifampin 300 mg bid and Vancomycin 1500mg ivpb q 12h. He was extubated on April 30th. Once extubated, he was placed on morphine for pain control. He was eventually switched from MS by patient controlled analgesia (PCA) to Oxycodone/APAP 5/325 2 tabs po q 6h and ibuprofen 800 mg 3-4x daily. Chip experienced a seizure on May 15 and was placed on Dilantin 100 mg tid. By May 17th he complained of tinnitus and an audiology consult was obtained but records cannot be found.
Care in Germany included: external fixation of the compound, left mid-shaft fracture; observation and monitoring for pulmonary contusion complications and resolution; antibiotic treatment for pneumonia and osteomyelitis; dental evaluation for broken teeth, reconstructive repair of left pinna; monitoring for head injury; and debridement and wound care for superficial lacerations, contusions, and abrasions. Brain MRI revealed left frontal-temporal-occipital punctate hemorrhages.
PMH:
Childhood ills: mumps, chickenpox, and croup.
Adult Ills: No HTN, DM, renal or pulmonary concerns, no hyperlipidemia
Medications: none, except daily multivitamin, occasional melatonin for sleep and Echinacea when he feels cold signs and symptoms
Allergies: NKDA
Immunizations: Td 4/19/11 Afghanistan
Past Surgical Hx: Appendectomy age 12, squamous cell carcinoma mole removed, left cheek 2002, no sequellae, external fixation of left compound femoral fracture, left pinna reconstruction, multiple dental extractions, debridement and wound care.
Family Hx: MGF (maternal grandfather) died, age 87 with CVA (Cerebrovascular accident), HTN (hypertension); MGM (maternal grandmother) alive at age 92, no known illnesses; PGF (paternal grandfather) died age 56 in coal mine collapse; PGM (paternal grandmother) died age 76 with CVA, DM (diabetes mellitus), and HTN. Mother alive, age 74 with hypothyroid, depression. Father alive, age 76 with HTN, hyperlipidemia, and gout. No siblings. 3 children without illness.
Social Hx: Married, heterosexual, works as a war correspondent. Denies tobacco or illicit drug use, occasional ETOH (1-2 glasses of red wine each night when not travelling)
Religion: agnostic
PE:
General: adult male with recent weight loss, (approx 40lbs)
Mental Status: Awake, alert, and oriented to time, place, and person.
Vitals Signs: Wt: 88Kg/195lbs” Height: 72” Pulse: 86 Respiration: 10 BP: 116/76
HEENT:
Cranial nerves: 3-12 are grossly intact with possible right visual field cut in cranial nerve 2 Ears: Left Pinna with 3cm sutured laceration-wound edges well approximated, no d/c, and no redness. Left tympanic membrane perforated no d/c or swelling in EAC (external auditory canal), Right TM pearly gray and mobile, no swelling or d/c in EAC. Unable to test hearing at this time.
Eyes: No periorbital edema or bruising, lids atraumatic, PERRL, conjunctiva- white, non-injected, non-erythematous; EOM grossly intact
Nose: Nares patent, no bleeding or d/c, septum midline.
Mouth: Several broken teeth left upper and lower jaw, tongue atraumatic, pharynx non-erythematous.
Face: no palpable deformities in mandible or facial bones
Neck: Trachea midline without shift; thyroid non-palpable, carotid upstrokes normal bilaterally without bruits
Chest: Lungs bilaterally clear to auscultation. No areas of tympany or dullness noted.
Cardiac: RRR, no S3, S4, or murmurs. PMI at the left 5th intercostal space with no palpable thrills.
Abdomen: Bowel sounds present in all 4 quadrants- soft, non-tender, and without rebound or guarding, or distension. Tympanic. Liver percussed at right mid-clavicular line and found to be within normal limits. No organomegaly noted. Rectal exam- normal sphincter tone, empty vault and hemoccult negative.
Back: No obvious injury, malformation, or deformity of the back. No costovertebral angle tenderness noted bilaterally.
GU: Normal adult male; circumcised, testes palpable without masses; no discharge or lesions noted. Rectal: prostate: symmetric, no nodules
LUE: No apparent deformities or fractures, full PROM, intact equal pulses, no edema.
RUE: No apparent deformities or fractures, full PROM, intact equal pulses, edema evident.
LLE: External fixation of a mid-shaft of the femoral fracture. Noted erythema of several pin insertion sites. Wound site closed with mild erythema and no drainage. Distal pulses intact, symmetric at 2+/2+. DP/PT pulses bilaterally equal. Skin of distal extremity exhibits normal color and temp. Restriction of passive ankle dorsiflexion, knee extension, and hip extension.
RLE: No apparent deformities or fractures, full PROM, intact equal pulses, no edema.
Dx Studies from Acute Care Medical Hospital in Germany:
1. CT revealed linear, non-depressed left temporal fracture without displacement
2. MRI revealed diffuse punctate hemorrhages in left frontal, temporal, and occipital regions
3. Post-operative plane films (multiple views) showed good alignment of left femur fracture with external fixation
4. Pulmonary function tests and radiologic studies revealed a pulmonary contusion which has since healed
5. CT of cervical spine revealed no abnormalities
Impression:
1. S/p head injury with multiple punctate hemorrhages
2. S/p left temporal fracture- non-displaced and healing
3. S/p pulmonary contusion, pneumonia-resolved
4. Compound fracture, mid-shaft, left femur-externally fixed- POD #60
5. MRSA wound infection and osteomyelitis-Rifampin and Vancomycin day# 56
6. S/P left parietal scalp laceration
7. Perforated Left TM
8. S/p laceration, left pinna- reconstructed
9. Abrasions- left face, left chest, left scapula, left flank/abd, left leg-healed
10. Pain and restriction of multiple joints of left lower extremity
12. Seizure-Dilantin day
13. Multiple tooth extractions
Plan:
1. CXR, AP and lateral left femur, EKG, CBC, CMP, UA, Dilantin level
2. Continue neuro monitoring for 24 h
3. Maintain IV access
4. Place PICC Line
5. Audiology consult
6. Dental consult
7. Physical therapy consult
8. OT consult
9. Percocet 5/325mg 2 po q 6h prn
10. Ibuprofen 800 mg 3-4x daily
11. Dilantin 100mg tid
12. Vancomycin 1500mg q 12 h
13. Rifampin 300 mg bid
Osteopathic
Admission Osteopathic Palpatory Evaluation
Gila Hospital Inpatient, Tucson, AZ
6-24-11
This additional information was obtained during the initial medical history and physical if done by a member of the osteopathic profession.
Head: Left temporal restriction, left occipital condylar compression, sphenobasilar synchondrosis restriction.
Cervical: Increased suboccipital muscle tone bilaterally; C2Rl; C3FRrSr; C5ERrSr; cervicothoracic compression bilaterally; tenderness distal left sternocleidomastoid.
Thorax: Elevated left clavicle; elevated left rib 1; decreased sternal motion during inhalation; T4ERlSl
Ribcage: Restriction ribs 6-9 on the left; depressed ribs 11, 12 on the left
Lumbar: Increased tone of the left iliopsoas and quadratus muscles; anterior counterstrain tenderpoints L1-4 left; lumbosacral compression; left iliacus tenderpoint; increase paravertrebral muscle tone left greater than right
Abdomen: Increased left oblique tone
Sacrum: Deep left sulcus, inferior R ILA
Pelvis: Inferior left ASIS, superior left PSIS, tenderness at the pubic tubercle bilaterally
Upper extremities: Tenderness left corocoid, left pectoralis minor tenderpoint
Lower extremities: Restriction left hip flexion, left knee flexion, left ankle dorsiflexion.
Impression: Additionally see medical H and P for this facility
1. Multiple somatic dysfunctions of the head, cervical, thorax, ribcage, lumbar, sacrum, pelvis, abdomen, upper and lower extremities.
2. S/p open femoral fracture treated with external fixation-currently undergoing rehab
3. Ruptured TM with hearing loss
4. Dental extractions
5. Gait disturbance
6. Seizure disorder-controlled
7. S/p osteomyelitis, head injury, temporal fracture, pneumonia, pulmonary contusion
Plan:
1. OMT1- 2x weekly to decrease pain, increase mobility, and quicken healing
2. Continue med/surg
3. Continue PT, OT, meds
Nursing
SBAR Report Nursing - Gila Hospital
Jones, Charles Robert (Chip) MRN: 593231
Date: June 25, 2011
38 year old Male
Admitting physician: Dr. Smith
Code status: Full Code
Allergies: NKA
Weight: 106.8kg/ 235lbs at time of injury Height: 6’ / 72”
Now: 88.63kg/195 lbs
Admitting Diagnosis: Trauma
Brief History of hospital course: Riding in a Humvee as a civilian photojournalist with the Marine Corp, struck by improvised explosive device (IED). Sustained serious injuries to left side of body including arm, leg, chest, and head/face. Spent time in Landstuhl Regional Medical Center, Germany prior to this admission.
Family/Social Concerns: Wife, Nancy and 3 children under 10 living in Tubac, Arizona
His parents live in Tucson, and wife’s parents live in Tubac. Patient is a photo journalist.
Contact precautions: MRSA in Left leg wound.
Clinical Assessment
Body SystemNeuro: |
InterventionExplain procedures and care items slowing for understanding Bed rails up x 2, call bell within reach, bed low and locked. PT MS Contin 30mg Q12 hours scheduled |
ResponsePatient able to follow commands. Pt did not experience a fall. |
| Respiratory: Upper anterior lungs-clear and equal Lower anterior lungs-clear diminished Upper posterior lungs-clear and equal Lower posterior lungs-clear diminished Lung expansion-equal bilaterally Breathing pattern-equal Sao2- 96 |
Encourage use of IS 10 times per hour |
Patient compliant with instructions. Lungs sound clearer. |
| Cardiac: Heart Rhythm-Regular Heart Rate-86 Cap Refill- >3 all extremities Turgor - good Radial pulses-strong right, slightly diminished on left. Dorsalis pedis pulses-strong right, slightly diminished on left. |
Continue to monitor pulses for changes |
| GI/GU: Bowel Sounds-active Abdomen-soft, rounded, non tender Urine-clear yellow Stool- Last BM -2 days ago in Germany Drains-N/A Diet- Regular Feedings-N/A |
Gave prescription BCOC |
Stool still pending |
| Integumentary / Musculoskeletal Lips: moist/pink Mouth: moist/pink Color: light pink undertones Texture: smooth Incisions: external fixater on L leg, pins clean and intact. Dressings: Scars: Ears: Patient complains of deafness in left ear. |
Pin cleaning daily Speak towards patient right side. |
Sites look free of infection Patient is able to hear and understand |
| Lines: Peripheral- 20 in RAC Central-PICC in RUE double lumen |
10ml Flush 10ml Flush per line |
Patent Both lines patient and positive blood return. |
| Vitals: Vitals HR 86 BP 130/70 Temp 98.6 RR 16 SAT 98% on room air |
Functional Health Patterns
Health Perception/Health Management
Subjective: Patient states “I just have no energy to try to get through all this health care to get better”
Objective: Patient tires easily when attempting to do physical therapy, occupational therapy or basic ADL’s.
Values and Beliefs
Subjective: Patient states “My family is very important to me and that is what keeps me going”
Objective: Patient smiles when he speaks about his family and watching his children grow up.
Cognitive/Perceptual
Subjective: Patient states “I normally learn by hearing, but since my hearing is bad, I have taken to seeing to learn”
Objective: Patient learns by seeing how to do things and questions things over and over due to his hearing loss.
Nutrition/Metabolic
Subjective: Patient states “Food just doesn’t taste the same with all the medications I’m taking and I have lost my appetite. Nothing sounds good”
Objective: Patient is encouraged to take in supplemental drinks to help with nutrition.
Activity/Exercise
Subjective: Patient states “ Before I got hurt I used to jog everyday for 2 miles”
Objective: Although tired patient is willing to work with physical therapy.
Elimination
Subjective: Patient states “I feel that my elimination was normal prior to the accident but now I have to take medications to have a regular pattern”
Objective: Patient is given medication for constipation on a regular basis and complains of constipation often.
Sleep/Rest
Subjective: Patient stated “Prior to the accident I slept 6 hours per night and never felt sleepy during the day. Now I feel like I can sleep all of the time.
Objective: If patient is not engaged with visitors or hospital staff he is sleeping
Role/Relationship
Subjective: Patient stated “I was the head of household when I would be at home and not traveling on assignment. My wife would then take over the role. Now I feel she will always be in charge, and right now I am okay with that”
Objective: Wife discusses issues with her husband but seems to hold back on some things due to fear of upsetting her husband and has expressed this to the nursing staff.
Coping/Stress
Subjective: Patient states “I’m so stressed with being injured and not being able to handle the stress of life outside of here in the hospital working on getting better.”
Objective: Patient seems to be sad at times when his family leaves after visiting
Self-perception/Self concept
Subjective: Patient states “I feel like I am out of control of my personal life and my family life since the accident. Prior to that I was very in control of my emotions”
Objective: Patient sometimes gets frustrated when trying to do things for himself.
Sexuality/Reproduction
Subjective: Patient stated “I do not feel comfortable discussing this subject”
Objective: Patient blushed when asked the questions.
Occupational Therapy
Occupational Therapy Initial Evaluation
Gila Hospital Inpatient
Date: 6/26/11
S: Client snoring loudly as OT entered the room. He did not initially arouse with verbal prompts but did open his eyes and visually track therapist intermittently when OT rubbed either arm vigorously and loudly called out his name.
0: Orders for OT received. Pt is 38 yr old male transported to this facility from Germany on 6/24/11 due to traumatic injuries suffered from an IED in Afghanistan. Chart reveals pt suffered multiple injuries primarily to L arm, leg, chest and face, with closed L temporal occipital puctate hemorrhages. TBI. PT saw pt earlier today and will address endurance and mobility problems. He has had surgical repair of L temporal skull fracture. Pt has external fixator to L femur due to multiple fx and is now TTWB L LE and Mod A for sliding board transfers according to PT notes. He was extubated on 4/30/11. Has recent hx of MRSA. Was tx for pneumonia which has now resolved. OTR began brief eval, with pt supine in bed, limiting it in order to avoid over stimulating pt, who has been agitated and intermittently combative with nurses when they attempt to back off sedation and pain meds. OTR provided PROM to shoulders, elbows, wrists and digits. Some abnormal increased flexor tone noted throughout R UE R hand is edematous especially at MCPs When asked to show how he would comb his hair, he did begin to grasp a hairbrush and raise it toward his head but was unable to complete that motion. Wife, Nancy is present and willing to provide background info but has excused herself from the room numerous times to answer cell phone and explained that she is getting multiple calls from relatives who are attempting to care for their 3 children. OTR explained the purpose, goals, and methods of OT to wife and she agrees that it is needed and wants to proceed as recommended by OTR. She feels he is unable to stay awake because he is being given too much Percocet and she says she has talked to the nurses about this and hoping they will decrease the dose. OTR instructed wife in how to perform retrograde massage to R UE in order to decrease R hand edema, and she gave good return demo and expressed willingness to perform regularly in order to reduce edema. OTR encouraged her to approach him from various positions around the bed in order to encourage him to sustain visual attention. OTR provided wife with the Modified Interest Checklist and she agreed to complete it in the next few days. OTR placed a large clock and calendar on the wall at midline in front of his bed. Pt did begin to become agitated but at that point, pts wife Nancy spontaneously sang a song to him and he calmed and smiled slightly. The following problems are identified by OT:
1. Pt requires max A for dressing, bathing, grooming, mouth care, feeding 20 to attention span of less than 1 min, SOB, probable pain, poor visual tracking, and possible cognitive impairment and/or hearing deficit.
2. Pt requires max A for all IADL
3. Risk of UE contractures due to probable pain, edema and immobility
4. Activity tolerance for ADL limited to less than 1 min
5. Ability to attend to tx limted to less than 1 min.
6. Cognition specifics to be determined. Does attempt to follow 1 step commands
7. Impaired ADL due to decreased UE strength, endurance and ROM. (requires further eval to determine specifics)
8. Incomplete occupational profile due to pts inability to adequately attend and communicate.
Speech and Language Pathology
Speech/Language Therapy
Gila Hospital Inpatient – Tucson AZ
Initial Evaluation – 06/26/11
S: Order requested from physician for SLP assessment by recommendation from PT due to noted word finding difficulty and Dx of TBI. Order received. Pt assessed bedside in room.
O: Chart reviewed:
Hx: This 38yo male Pt sustained multiple injuries on 4/19/11 as a result of an IED explosion in Afghanistan while embedded with the U.S. military as a photo journalist. He was transported to an acute care hospital in Germany where he received medical care and therapy from 4/21 to 6/25/11. The Pt was admitted to this hospital on 6/25/11. Injuries included closed head injury (CHI); L tympanic membrane rupture; multiple contusions and lacerations/abrasions of L scalp, face, ear, flank, leg, shoulder, chest and abdomen; contaminated, open L mid-shaft comminuted femur Fx; broken teeth; and pulmonary contusion. Initially the GCS was 10 and he was placed in a medically-induced coma for transport to Germany and remained in coma state until 4/23/11. Intubated and ventilated initially and was extubated on 4/30/11. He was treated for L femur Fx. A CT revealed L temporal skull Fx and an MRI revealed frontal-temporal-occipital punctate hemorrhages. Pneumonia developed on 4/27/11 and is resolved; he is being treated for MRSA and osteomyelitis on L LE; he is on Dilantin due to seizure activity on 5/15/11; he has c/o of tinnitus and is being followed by audiology which reported L-ear mild-severe sensorineural hearing loss. It was also noted that the Pt has some R-visual field cut.
Social: The Pt is college educated and married with 3 children under the age of 10 and wife is extremely supportive. His parents and in-laws are within driving distance and are involved in his care.
Precautions: MRSA LLE, Hx of seizures, reduced attention span, R-visual field cut, decreased frustration level becoming agitated when overwhelmed.
Assessment:
Auditory comprehension – The Pt was able to follow simple 1-step directives with 100% accuracy, but had difficulty with complex and 2-step commands.
Verbal expression – Word finding difficulties were apparent during the interview with noted semantic errors (labeling an object with the name of a closely related object – i.e. table for chair). The Boston Naming Test (a test that measures confrontational word retrieval using line drawings). His score was reduced indicating an anomia. Conversational speech was telegraphic containing primarily nouns, a few verbs, and few “functor” words (non-content words).
Reading comprehension – The Pt was able to match word to picture, but reading test was discontinued due to Pt demonstrating frustration at effort to correctly match phrases to pictures.
Written expression – Testing was not completed at this time due to UE weakness and Pt’s poor attention span and fatigue.
Oral-motor examination – With the exception of dentition the Pt’s oral motor structures were WNL. Labial and lingual structures had normal ROM, tone, strength, and coordination for speech and swallowing. Speech and swallowing are WFL.
A:
The Pt demonstrates a moderate to severe aphasia characterized by anomia. Further examination is necessary when Pt is able to tolerate treatment for extended periods of time and is not so easily overwhelmed to determine cognitive abilities. Potential impact of R visual field cut will be assessed when the Pt is able to tolerate more complex reading activities.
P:
Goals:
1) Improve word recall skills in order to communicate medical and basic wants and needs.
2) Improve attention skills to accurately complete simple therapy over 5 min.
3) Improve auditory comprehension for 2-step directives in order to participate in therapy activities.
4) Complete assessment for reading comprehension and written expression.
Physical Therapy
Physical Therapy
Gila Hospital Inpatient, Tucson, AZ
Initial evaluation 6/26/11
S: Pt lying semireclined in bed, external fixator left (L) lower extremity (LE). IV.
O: History: Pt. admitted 6/25/11 from hospital in Germany where he was admitted from 4/21/11-6/24/11 for treatment of multiple injuries from an IED in Afghanistan 4/19/11. Injuries included, closed head injury (CHI); L tympanic membrane (TM) rupture; multiple contusions and lacerations/abrasions of L scalp, face, ear, flank, leg, shoulder, chest and abdomen; contaminated, open L mid-shaft comminuted femur fracture; broken teeth; pulmonary contusion. Glasgow Coma Score of 10 initially and patient in medically-induced coma for transport to Germany. Intubated and on ventilator initially, and extubated 4/30/11. External fixator applied to L femur fracture 4/24/11; fracture remained open for healing; wound now closed. CT: L temporal fracture. Brain MRI: L frontal-temporal-occipital punctate hemorrhages. Developed pneumonia 4/27/11 (resolved); MRSA and osteomyelitis (on Vancomycin) L LE; seizures 5/15/11 (on Dilantin); c/o tinnitus.
Social: Married, 3 children, works as a photo journalist.
Precautions: MRSA L LE; History of seizures; Toe-touch weight bearing (TTWB) L LE.
Examination findings:
Cognition/language: Alert, oriented to time, place and person. Consistently follows simple verbal instructions, but occasional problem with complex verbal instructions. Utters several words appropriately in response to questions, but sentences are incomplete.
Sensation: Difficult to test sensation due to language impairment, but light touch appears intact right (R) upper extremity (UE), R LE, L UE, and distally L LE. Responds to stimuli presented in L visual field more often than when presented in R visual field
Motor: PROM intact R LE, L UE, R UE except mild limitation R MCP flexion and edema MCPs; L LE: Hip flexion 10-90 degrees, knee flexion 10-70 degrees, ankle dorsiflexion -10 degrees.
Tone: Mild increased flexor tone R UE and mild increased tone R plantarflexors, otherwise normal.
Strength: R UE 3/5, R LE 4/5, L UE 5/5; L LE: 3+/5 hip flexion, 3+/5 knee extension, 4/5 ankle dorsiflexion/plantarflexion. Pain 5/10 rating on PROM/AROM L knee.
Balance: Able to perform simple functional activities sitting at edge of bed with supervision and no loss of balance. Maintains standing with FWW, TTWB L LE with minimal assistance.
Mobility: Minimal assistance moving supine to sitting at edge of bed. Maintains sitting at edge of bed with supervision. Moderate assistance for sliding board bed, chair, commode transfers, transferring to R. Modified independence manual wheelchair propulsion 300’ level surfaces; supervision for propelling wheelchair on minimum grade ramps. Able to tolerate sitting for 90 minutes before requesting to go back to bed. Ambulation with FWW 150’ level surfaces with minimal assistance, TTWB L LE. Moderate assistance up and down one 6” step with FWW.
A: Major impairments and activity limitations include:
1) Occasional word finding problems. Consistently follows simple verbal instructions, but occasional problem with complex verbal instructions
2) Possible R visual field cut
3) R UE and LE weakness
4) L LE limited PROM, strength and pain due to femur fracture
5) Impaired balance in standing and walking
6) Limited endurance
7) Minimal to moderate assistance for all mobility. TTWB L LE
Goals:
1) Increase strength R UE and LE to 5/5 for increased use in ADLs.
2) Increase PROM R knee flexion to 80 degrees flexion, R hip and knee extension and R ankle dorsiflexion to neutral (0 degrees).
3) Supine to sitting with supervision.
4) Sliding board transfers to bed, chair, commode with minimal assistance of 1.
5) Tolerate sitting up in wheelchair at least 2 hours.
6) Modified independence manual wheelchair propulsion on minimum grade ramps.
7) Ambulation with FWW 300’ level surfaces with supervision, TTWB L LE.
Plan: Therapeutic exercise and mobility training 1-2x/day.
Dental
Gila Hospital In-patient, Tucson, AZ
Upper/ Lower impression made
Fabrication of interim upper partial to replace missing teeth
