 Mr Yoder was admitted to Blessing Hospital, Quincy with a diagnosis of sepsis.
Mr Yoder was admitted to Blessing Hospital, Quincy with a diagnosis of sepsis.
Blessing Hospital is the largest medical center in a 100-mile radius of Quincy, with a medical staff of more than 240 physicians and a team of more than 2,000 employees.
Blessing Hospital’s website describes it as the regional leader in patient and family centered care, Blessing Hospital is committed to excellence. Offering quality, compassionate and comprehensive medical care, and places a strong emphasis on community wellness. Blessing continues to respond to the changing health care needs of the region’s residents by keeping pace with technology and providing services that are convenient, accessible and vital to the mission to improve life.
Case Notes
Nursing
Nursing Admission to Medical Surgical Unit
Gender: M Age: 80 Race: Caucasian Weight: 109 kg 240 pounds Height: 183cm 72 inches
Religion: Protestant Major Support: Jon (son) Phone: 869-555-3452
Allergies: No known allergies
Immunizations: Influenza last fall; tetanus – 4 years ago
Past Medical History: Diabetes Type 2 diagnosed July of this year.
History of Present illness: Complaints of fatigue. This patient had also developed an ulcer on his big toe 3 weeks ago. Has been soaking his foot to heal the wound; recently revealed the wound to his family.
Chief Complaint: Patient stated “I have pain in my big toe and my right foot”.
Social History: Widower; his son Jon lives nearby
Primary Medical Diagnosis: Diabetic foot ulcer, Type II diabetes, Sepsis
Current Medications: Metformin 1000mg PO BID; Insulin Lantus 10 Units SQ QD x 1 month; Benadryl 25-50 mg at HS prn insomnia; APAP 1000mg prn.
Surgeries/Procedures & Dates: L4-5 laminectomy – 25 years ago; transurethral resection of the prostate – 6 years ago
Hygiene and sleep patterns: Showers 2 to 3 times a week, oral care performed daily, sleeps approximately 5 hours per night with naps while watching tv during the day.
Alcohol/smoking/drug history: Client denies use of alcohol or illicit drugs. History of chewing tobacco for approximately 30 years. Client quit chewing tobacco 15 years ago. No history of smoking.
Educational data: Client denies the need for special cultural, dietary or religious considerations. Client states he learns best by doing. Risk for readiness to learn.
Functional Screen: Client currently lives alone and states “I’m having more trouble taking care of my house and myself each day that goes by”. Able to shower occasionally and dress himself with effort.
Fall Risk: High fall risk. Client unsteady on his feet and holds onto furniture to get around. No ambulatory aides are currently used.
Nutrition screen: Client states “I eat frozen meals as they are easy to prepare being alone. I don’t worry about what it is and am not worried about my diabetes”.
Nursing assessment day 1 - medical / surgical unit
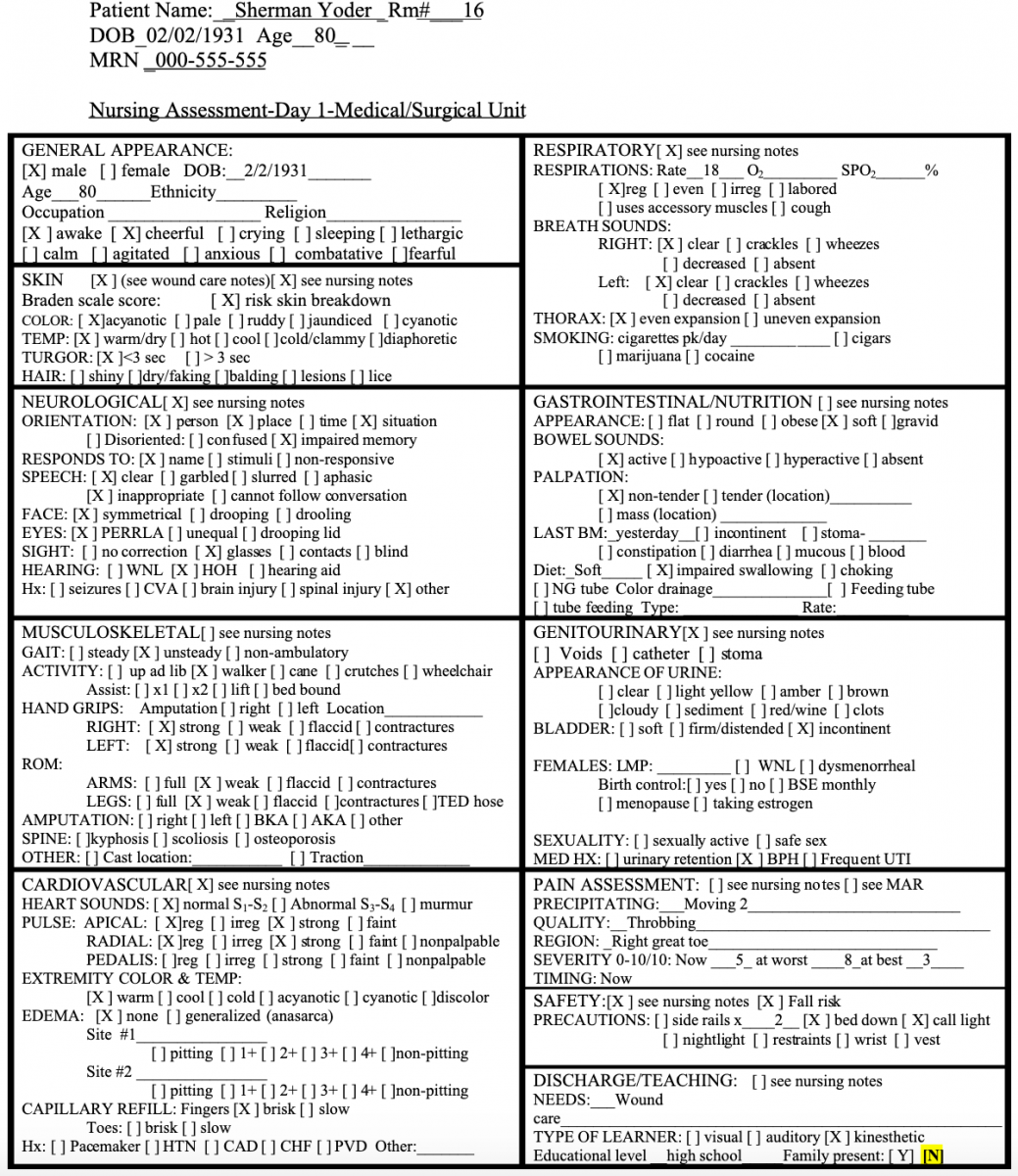
Nursing notes - Inpatient Day 1
Patient direct admit by doctor’s recommendation to obtain wound nurse evaluation of right great toe wound. Patient cheerful, talking and infusing 0.45 sodium chloride in right AC 20 gauge.
Nurse signatures
Initial Nurse Signature
NS Nancy Smith, RN
Nursing assessment day 2 - ICU
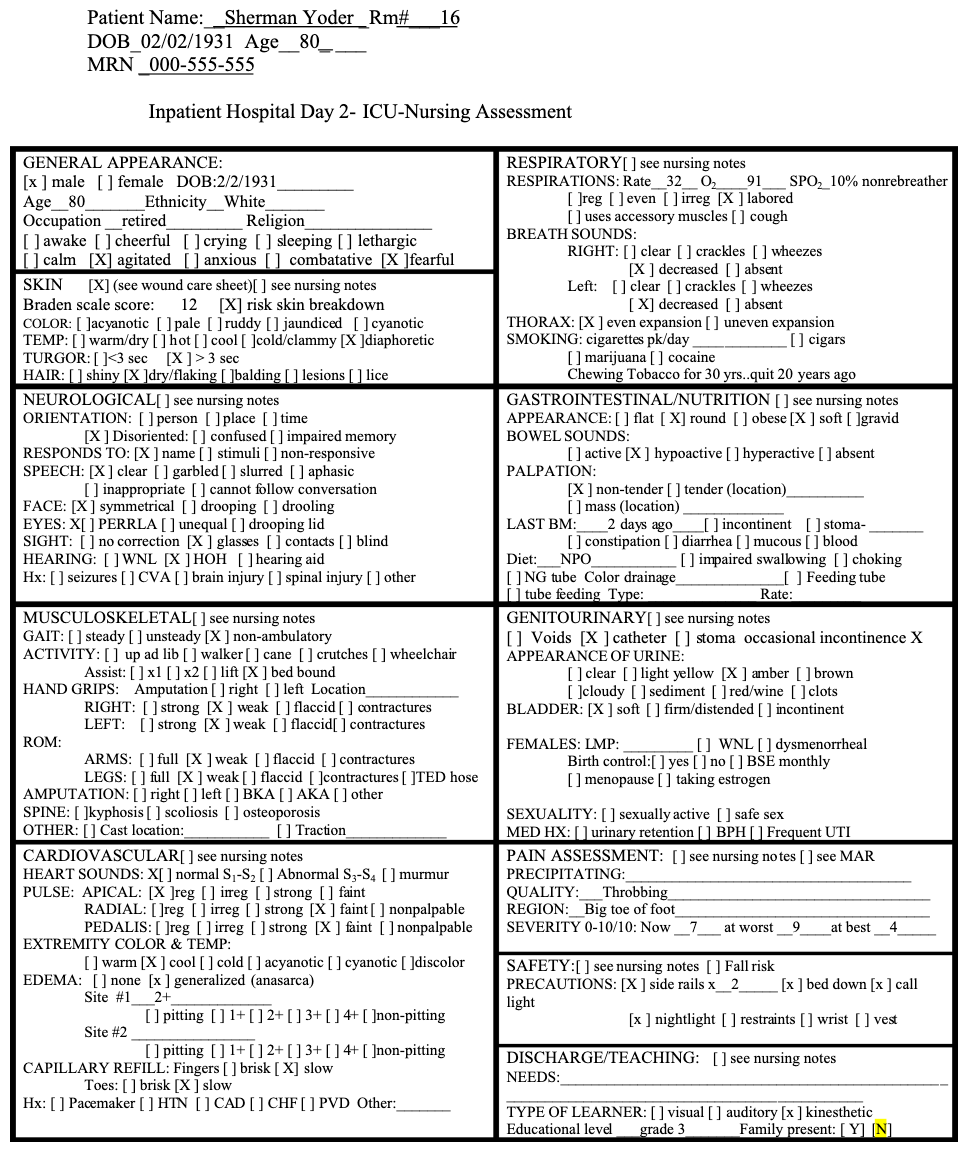
Nursing notes - Inpatient Day 2
Nurse signatures
Initial Nurse Signature
NS Nancy Smith, RN
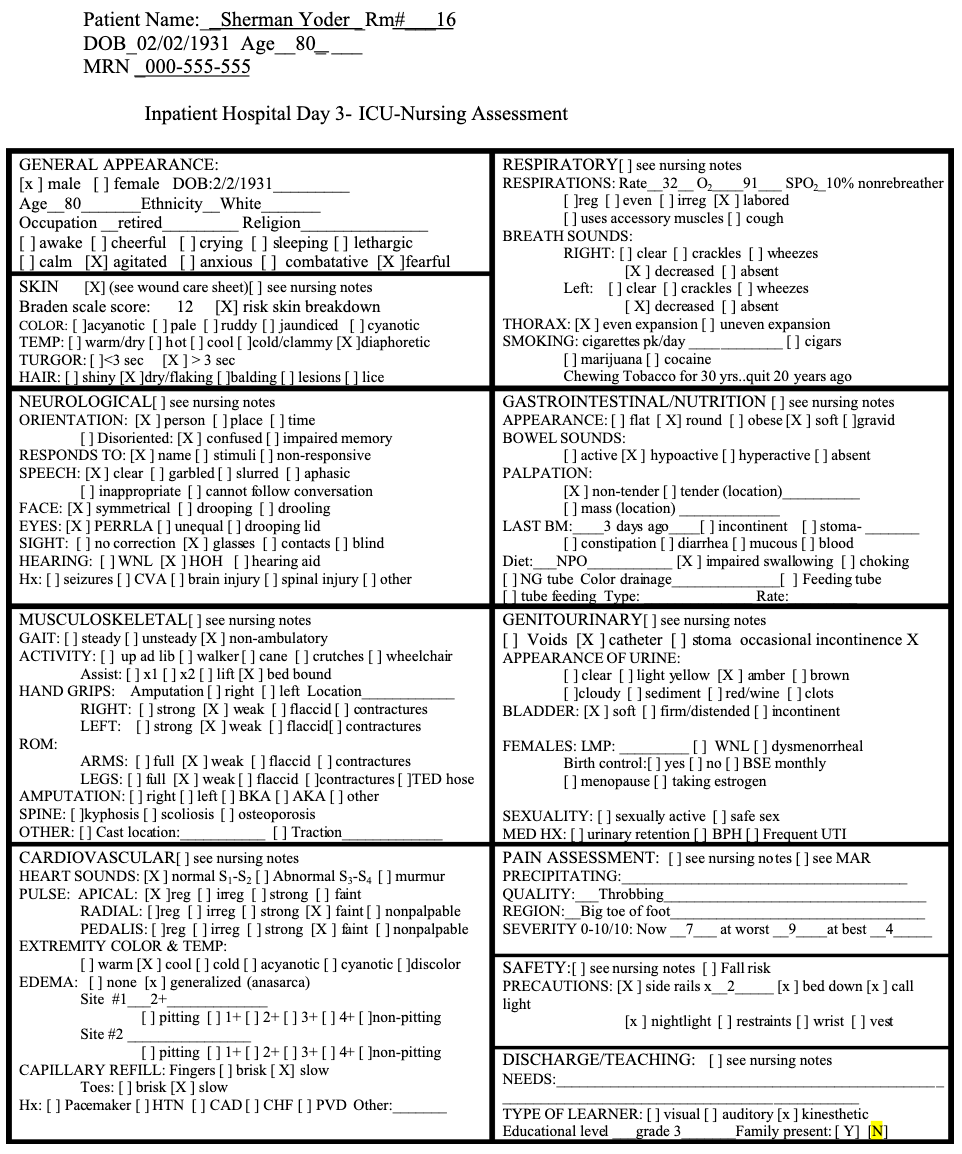
Nursing assessment day 3 - ICU
Nursing assessment day 4 - medical/surgical unit
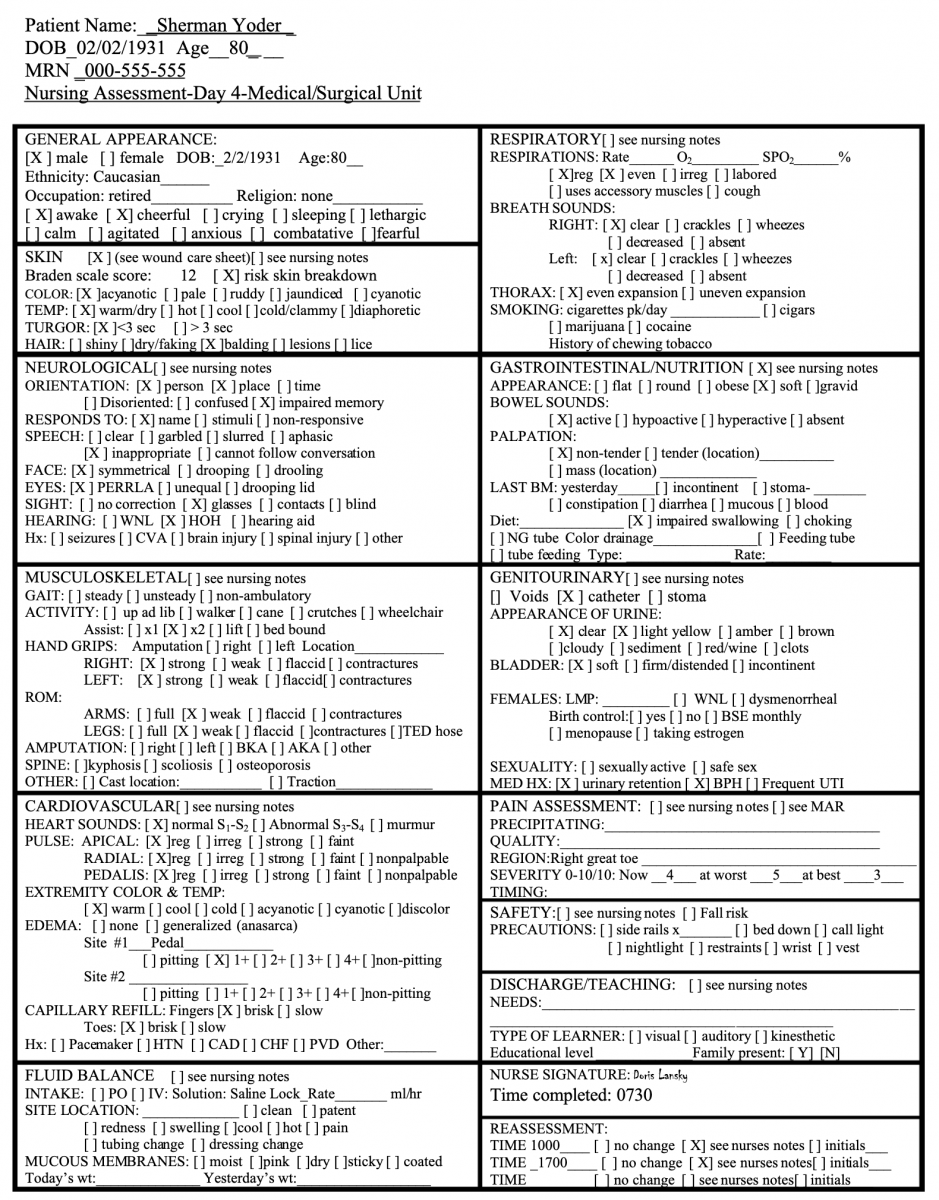
Nursing notes - Inpatient day 4
Nurse signatures
Initial Nurse Signature
DJ Diane Jones, RN
Nursing assessment day 5 - medical/surgical unit
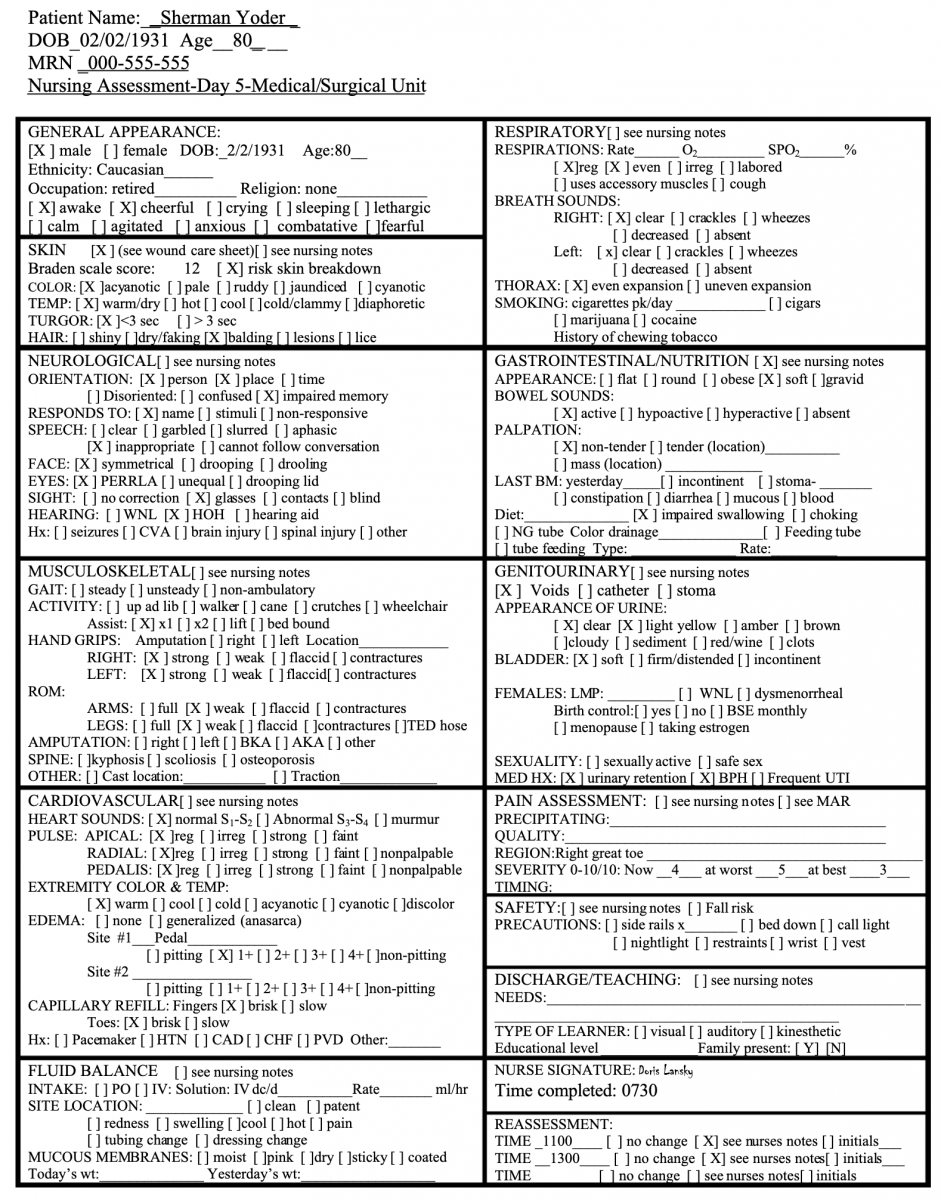
Nursing notes - Inpatient day 5
Patient direct admit by doctor’s recommendation to obtain wound nurse evaluation of right great toe wound. Patient cheerful, talking and infusing 0.45 sodium chloride in right AC 20 gauge.
Nurse signatures
Initial Nurse Signature
NS Nancy Smith, RN
Occupational Therapy
Reason For This Admission: Open wound R great toe, Sepsis, IDDM
PMH: L4-L5 Laminectomy aprox 1990, Prostate surgery/TURP , aprox 2008
Occupational Therapy Initial Evaluation
O: OTR/L began eval after reviewing chart. According to nursing notes pt is here to be treated due to R great toe open wound and sepsis. He was DX with IDDM aprox 6 months ago and is on insulin. He is described as A & O, conversant, able to drive, and living alone with some help from son, Jon and daughter in law Judy who live near his farm outside Edina Mo. OT eval was requested by Judy, who is questioning his ability to live by himself.
Perception Pt wears bifocals. He had no difficulty following conversation and expressed himself with ease. No word finding issues were observed. Pt does not use hearing aids.
Cognitive: Pt scored 24 out of 30, suggestive of mild cognitive impairment, on the MOCA with 2 points lost for concrete responses regarding the abstraction subtest. Pt has a high school education.
Sensation: UE sensation is intact. Pt does complain that he has to fumble for things like coins and keys.
Strength/ROM: UEs WFL and pt has no complaints.
ADL: Nursing notes indicate he scores “6” on the KATZ. OTR performed the Kohlman Evaluation of Living Skills administered through interview and direct observation of actual abilities. Pt scored as Independent in health, money management, transportation, telephone and leisure and needs assistance in areas of daily activities in self care, safety and health. Pt is I with feeding. He denies problems with chewing, choking or swallowing, but states that his tongue has felt different lately. Pt is I with toileting but c/o prbs with reaching to wipe and so OTR instructed him in some alternate techniques to support and elongate the spine and pt agrees he will practice and let therapist know his success. Pt c/o intermittent sleep problems and attributes them to prbs getting physically comfortable due to pain in his feet and legs at times that he rates as a “5”.
Mobility: Pt is using a FWW in an attempt to keep weight off the toe and relieve pain, but admits he actually is finding it helpful. As determined by PT eval, if he will be continuing with FWW, he may benefit from obtaining a walker tray or basket in order to transport items. He arose easily from the bed, chair and toilet.
Psychosocial/Family: During OT eval, pts son John visited briefly on his way to work. OTR advised him that Mr Yoder will likely need some adaptive equipment in order to improve his safety with ADL. John stated he does not know when he can get to that issue and expressed frustration with his dad’s needs for assist….”Holy Cow!….we already stop by there about every other day as it is! Our own lives are turning to CRAP, and it looks like my son is going to get kicked out of college or at the very least lose his scholarship….and now THIS! I don’t know how much of this SHIT I can take…I’m about done. We’re going to have to talk about this more later….here Dad….I brought you the paper….I gotta go…..sorry.” After John left, the pt apologized profusely for his behavior and admitted it has gotten worse and worse lately to the point that Mr Yoder avoids bringing up issues that he knows will create more work for John or Judy. Mr Yoder denies that there is anything more than shouting and specifically denies that John has ever hurt him. Pt accepted the offer of leaving an adaptive equipment catalog with the specific items that might help him circled and he said he planned to talk to John about it later, “after he cools off”.
A: The following issues will be addressed by OT:
- Pt requires SBA during bathing due to safety risk and admits to falling 2x in recent months when he arose quickly to answer the door or phone. Pt sates he has no adaptive equipment in the home and has been a bit scared about bathing on his own and so has recently resorted to just sponge baths at the sink.
- Pt requires MIN A for LE dressing due to decreased ROM of his lower back with residual decreased sensation of R LE, RT to laminectomy and or neuropathy. Pt has no adaptive equipment and admits he does not change his socks daily because he is unable to get them on.
- Impaired communication/family support system.
Goals For OT:
- Pt will demonstrate safe Shower with adaptive equipment within 1 wk.
- Pt will demonstrate I LE dressing using adaptive equipment and techniques with 1 wk
- Determine specific unmet needs of client and explore community resources to reduce caregiver burden
Strengths:
- Cognitively intact
- Involved family
OT Planned Interventions: OT 1x day x 7-10 days
- OTR/L will further assess for potential to benefit from use of tub transfer bench, long handle scrub sponge and bath mat. Will provide safety training.
- OTR/L will provide instruction in use of dressing stick, sock donner and long handle shoe horn for LE dressing. Will encourage regular skin inspection using long handle mirror.
- Request MSW eval to explore community resources that may reduce caregiver burden and to explore ways to improve communication/rapport between pt and son.
DC Plan: Dc in 1-2 weeks or when goals met. Pt will benefit from home health OT to insure carry over to his own home situation, evaluate his safety in his own natural environment, and to help family adjust to his new status. Evaluation of meal prep would be most effective in his own home. Pt might benefit from meals on wheels, the friendly visitor program, or other ways to expand his social circle and support beyond his own family.
Olivia Opres, OTR/L
Progress Note, Next Day
S: “John stopped by last night after work and he had cooled off by then. I do think he will help me get the equipment, but he couldn’t believe that Medicare won’t pay for that stuff when it is obviously needed.”
O: OTR.L began ADL/safety training using sample adaptive equipment including a tub transfer bench, long handle scrub sponge, reacher, sock donner and dressing stick. OTR/L advised him to back up to the tub transfer bench, using the walker, and sit down first, then swing his legs over the edge of the tub, and remain seated throughout the shower. OTR allowed pt a 30 min rest in bed then returned to resume dressing training with pt sitting in chair near the bed. Pt has now been seen by PT and has been advised to continue with FWW and has recommended using an off loading shoe. Pt is expressing concern about how that will work out when he needs to get in the hen house to collect eggs. OTR encouraged him to discuss with the PT.
A: Progress toward goals:
- Pt demonstrated ability to perform shower from seated position on tub transfer bench with verbal cues and he is convinced that obtaining the same thing will help him. He is impressed with the advantage of not needing to step over the edge of the tub anymore and is relieved to know that he will not likely need any bathroom renovations if he gets the bench which will cost aprox $100.00.
- Pt was fatigued after the shower but benefitted from the ½ hour rest before attempting LE dressing. He states in the past he has made a point of trying to hurry through the shower and dressing and this caused him to feel fatigued and sometimes even SOB, but had led Judy and John and even the nurses to believe that he was showering regularly without difficulty because he did not want them to think that he also needed assist with that. Pt will require more practice with the sock donner to be fully independent.
- OTR/L suggested the possibility of pt receiving home health to evaluate him in his own home and make sure that he was safe there, and pt was receptive.
P: Continue with plan as outlined in initial eval. Introduce concept of energy conservation next tx. Check with physical therapy re pts mobility needs and if it is likely that he will be sent home with a walker or not. MSW has been to see the pt according to nursing notes, but MSW note was not in the chart yet.
Olivia Opres, OTR/L
Psychology
CLINICAL HEALTH PSYCHOLOGY
Met for initial evaluation to assist Mr. Yoder in the adjustment to his medical condition and to assist the team in determining Mr. Yoder’s capacity to manage on his own at home. OT noted some possible cognitive impairment on administration of the MOCA and nursing has noted increased cognitive impairment later in the afternoon. His son, Jon Yoder, has reported frustration with his father’s “continuing to ignore the doctors” and poor judgment in realistically dealing with his home environment. There are also reports of problems with sleep and chronic pain, and daily use of alcohol.
Mr. Yoder agreed to assessment and signed the Informed Consent after being told the limits of confidentiality. He reported understanding that the information obtained would be shared with his healthcare team.
Background Information: Mr. Yoder is an 80-year-old, widowed Caucasian male who lives independently in rural Missouri, where he has lived all of his life. He is a Korean War veteran. His wife of 50 years died 10 years ago. He has one son, Jon, and a daughter-in-law, Judy, who have children and live locally. The oldest grandson, Jack, is away at college studying agronomy. Judy is a nurse assistant at a local nursing home. Mr. Yoder’s son has a part-time job and helps run the farm. Mr. Yoder has been a farmer all of his life, having taken over the farm when his father died. He has siblings who, according to Mr. Yoder, “left the land as soon as they could,” but it is not clear if he has any interaction with them at this time. His son and daughter-in-law currently help him to continue to live independently and to maintain the farm.
Socially, Mr. Yoder appears to continue to be engaged with the community where he has lived all of his life. He is active with his church and meets friends weekly at the Veterans of Foreign Wars (VFW) hall for coffee and doughnuts. He reports “getting caught up on all the town gossip” and getting involved in conversations about world events.
Medical History: Mr. Yoder reports “being stiff in the morning” and having been diagnosed with diabetes six months ago. He is ambulatory and drives. He has a regular health care provider, Dr. Bake. Mr. Yoder reported initially taking oral medication for diabetes and is currently being on insulin. His commitment to the dietary management of his diabetes is a problem, as he reports that he is “not going to live forever” and “should be able to eat what he wants.” Recently, problems resulting from his poor diabetic management include a sore on his foot that is not healing.
Mr. Yoder reports problems with sleep, stating that he “has not slept through the night for years.” He reports that “even the couple of beers I have at night ….don’t seem to help any more.” He reports currently using Benadryl to help him sleep. It is not clear if he is using the Benadryl in addition to the alcohol.
Mental Health History: Mr. Yoder denied any prior mental health problems or treatment. He did endorse a long-term history of sleep problems and having “a couple of beers” daily. He denied alcohol use having ever been a problem and that he would have no difficulty discontinuing use of alcohol. However, as with his dietary management, he reports that he is “not going to live forever” and should be able to eat and drink what he wants.
Summary: Mr. Yoder is an 80-year-old Caucasian male who suffered the loss of his wife 10 years ago and is currently dealing with significant stressors in regard to chronic disease management and maintaining the social support needed to remain independent. There are concerns regarding his capacity for complex decision making, which may be influenced by his chronic sleep problems and regular use of alcohol. In addition, his self treatment for sleep problems with alcohol and Benadryl has the potential to impact his overall well-being, including increased risk for falls and impairment in cognition and mood.
Recommendations:
Full cognitive and mood assessment to rule out dementia/pseuodementia and to establish full competency for complex decision-making.
- Evaluation of chronic sleep problems to determine etiology and to rule out the possibility of undiagnosed Post Traumatic Stress Disorder.
- Identify a provider who can administer an evidence-based behavioral sleep intervention (RESTORE, McCrae, 2007)to improve Mr. Yoder’s symptoms of insomnia.
- Evaluation of current and past history of alcohol use.
- Evaluation of Stage of Change (Prochaska & DiClementi) and use of Motivational Interviewing in regard to treatment compliance for diabetes and other health behaviors, including alcohol use.
- Follow-up counseling to assist with the implimentations of the recommendations and to support Mr. Yoder and his family.
DSM-5 Diagnosis:
331.83 (G31.84) Mild Neurocognitive Disorder (Provisional)
311 (F32.9) Unspecified Depressive Disorder (Provisional)
309.81 (F43.10) Post Traumatic Stress Disorder (PTSD) (Provisional)
291.1 (F10.99) Unspecified Alcohol-Related Disorder (Provisional)
780.52 (G47.00) Insomnia Disorder, persistent
Thank you for allowing me to participate in Mr. Yoder’s care.
Health Educator
Consultation 1: Diabetes and Diabetes Self-management
Health Educators/Health Education Specialists: Job Description
The U.S. Department of Labor Bureau of Labor Statistics (BLS) defines health educators (SOC 21-1091.00) as those who promote, maintain, and improve individual and community health by assisting individuals and communities to adopt healthy behaviors, collect and analyze data to identify community needs prior to planning, implementing, monitoring, and evaluating programs designed to encourage healthy lifestyles, policies and environments. They may also serve as a resource to assist individuals, other professionals, or the community, and may administer fiscal resources for health education programs. http://www.bls.gov/soc/soc_f1j1.htm
Health Education Specialist Responsibilities and Competencies
Area I: Assess Needs, Assets and Capacity for Health Education
Area II: Plan Health Education
Area III: Implement Health Education
Area IV: Conduct Evaluation and Research Related to Health Education
Area V: Administer and Manage Health Education
Area VI: Serve as a Health Education Resource Person
Area VII: Communicate and Advocate for Health and Health Education
Brief Video about Certified Health Education Specialists/Roles and Responsibilities: http://www.sophe.org/healthedspecialist.cfm
Brief Videos: What is Public Health/This is Public Health:
http://www.whatispublichealth.org/what/
http://www.thisispublichealth.org/video_lowres.html
—————————————————————————————————————————-
A. DIABETES MANAGEMENT – NUTRITION/HEALTH EDUCATION
Nutrition Assessment items
For diabetes knowledge (to inform education needs): Michigan Diabetes Research and Training Center Brief Diabetes Knowledge Test – pdf.
Screens for current diet - They are free online. The one specific to carbohydrate intake must be purchased, but these are still good for providing a snapshot of the patient’s diet.
Fruit/vegetable/fiber intake - http://www.nutritionquest.com/wellness/free-assessment-tools-for-individuals/fruit-vegetable-fiber-screener/
Fat intake - http://www.nutritionquest.com/wellness/free-assessment-tools-for-individuals/fat-intake-screener/
Nutrition Education item
Tips for meal planning:
Six Easy Steps to Create Your Plate
It’s simple and effective for both managing diabetes and losing weight. Creating your plate lets you still choose the foods you want, but changes the portion sizes so you are getting larger portions of non-starchy vegetables and a smaller portion of starchy foods. When you are ready, you can try new foods within each food category.
Try these six simple steps to get started:
1. Using your dinner plate, put a line down the middle of the plate. Then on one side, cut it again so you will have three sections on your plate.
2. Fill the largest section with non-starchy vegetables such as:
- spinach, carrots, lettuce, greens, cabbage, bok choy
- green beans, broccoli, cauliflower, tomatoes,
- vegetable juice, salsa, onion, cucumber, beets, okra,
- mushrooms, peppers, turnips
3. Now in one of the small sections, put grains and starchy foods such as:
- whole grain breads, such as whole wheat or rye
- whole grain, high-fiber cereal
- cooked cereal such as oatmeal, grits, hominy or cream of wheat
- rice, pasta, dal, tortillas
- cooked beans and peas, such as pinto beans or black-eyed peas
- potatoes, green peas, corn, lima beans, sweet potatoes, winter squash
- low-fat crackers, snack chips, pretzels and light popcorn
4. And then in the other small section, put your protein such as:
- chicken or turkey without the skin
- fish such as tuna, salmon, cod or catfish
- other seafood such as shrimp, clams, oysters, crab or mussels
- lean cuts of beef and pork such as sirloin or pork loin
- tofu, eggs, low-fat cheese
5. Add a serving of fruit, a serving of dairy, or both as your meal plan allows.
6. To complete your meal, add a low-calorie drink like water, unsweetened tea, or coffee.
Source: American Diabetes Association (2014) Create your plate. Retrieved from http://www.diabetes.org/food-and-fitness/food/planning-meals/create-your…
Nutrition Education Caregiver item
8 Tips for Caregivers
From Diabetes Forecast
By Lindsey Wahowiak
March 2014
A diabetes diagnosis can be overwhelming. As caregivers, we want to support our loved ones and help them enjoy the healthiest lives possible. But what is the best way to do that? We talked to experts—both health care providers and people who have been there—to learn what is helpful and what to avoid.
Start Your Education Now
Any diagnosis presents a learning curve. Your first and best step in becoming an ally for your loved one is to arm yourself with education, says Shantanu Nundy, MD, of Mary’s Center, a Washington, D.C., health care and social services center for low-income families.
Some people believe that diabetes is “not a big deal” or, alternately, that it’s a death sentence, so it’s important to know the facts. “As physicians, we try to debunk [misconceptions], but information coming from a trusted family member or friend is really powerful,” Nundy says. “[Diabetes is] something you can live a long, healthy life with, by managing it.”
You can ask your loved one’s health care provider about where to learn more, including books, online communities, support groups, and sites such as the American Diabetes Association’s diabetes.org.
The learning curve can be steep, says Stacey Simms, whose 9-year-old son, Benny, was diagnosed with type 1 seven years ago, but she says it has been manageable for her and him. “My advice is to take a deep breath and realize that the beginning is the worst,” Simms says. “Now it’s just our routine, and it will become yours as well, eventually.”
Take Some Time
You can learn things and make changes bit by bit, to avoid overhauling your lives based on a loved one’s diabetes.
Jessie Gruman, PhD, should know. She’s a psychologist and five-time cancer survivor who wrote a book on coping with a new diagnosis: AfterShock: What to Do When the Doctor Gives You—or Someone You Love—a Devastating Diagnosis. She suggests giving yourself and your loved one time to digest the information. “People are shocked, and they feel like their life has changed in these earth-shattering ways,” she says. “As we learn more, as time goes by, as we adjust, as we make decisions, the way we feel changes a lot.”
So don’t rush your loved one (or yourself) from mourning to acceptance. Instead of saying, “You’re not going to feel this way tomorrow,” it may be more helpful to say, “This is really scary. What are you most worried about?
Encourage Self-Care, but Don’t Be a Pest
There’s a fine line between checking in on someone’s well-being and what Gerald Strauss, PhD, a psychologist with the Veterans Affairs (VA) health care system, calls “miscarried helping”—also known as nagging.
“Though people really do want to help their loved ones with diabetes, this backfires and just sends people running in the opposite direction,” he says. Don’t pester: Explain what you would appreciate your loved one doing. Strauss suggests role-playing these requests with health care providers or a diabetes care team to make sure your approach will be well-received.
Of course, with children, you will have to supervise, so weigh how much they might be able to handle on their own, advises Anne Doyle, a member of the Diabetes Forecast Reader Panel. Her daughters both have type 1 diabetes. “Give them one task at a time, and give them time to be successful at it,” she suggests. “Also be ready to take some responsibilities back from your child if you see them struggling.”
Preteen and teenage children often need parental supervision to stay consistent with care.
Make Changes Together
Your loved one’s diagnosis probably means making some lifestyle changes. Going through that alone might feel isolating, so why not make the changes together as a team or household? Start exercising together or look for diabetes-friendly recipes together—then cook and eat them together.
“A lot of the things that improve the care for someone with diabetes are actually good for everybody,” Nundy says. “It’s always better than going it alone.” Nundy knows this firsthand: He’s helped his mom care for her type 2 diabetes.
Set Small Goals
Taking a step-by-step approach is the easiest way to make permanent lifestyle changes, says Elizabeth Koustis, RD, LD, of the VA. Doing small things, such as taking a walk after dinner, can improve blood glucose and overall diabetes management, and allow you to look at the results and reevaluate as needed. “I think that’s very motivating for the patient, and they can continue to move forward,” Koustis says.
Offer help only if you really mean it. Saying “let me do anything I can to help you” is so broad, most people won’t take you up on it. So be specific about what you’re able to help with, and offer only if you really can help, says Gruman. “There’s nothing harder than to ask for help and then have it refused,” she says. So can you give your loved one a ride to the doctor? Then offer that—it’ll be appreciated.
Work With the Diabetes Care Team
Attend doctor’s appointments and diabetes education classes together if your loved one agrees. Nundy suggests listening to what both health care providers and the patient are saying, chiming in with what you know, and asking questions to help your loved one get the best care possible. That includes making sure the health care team is complete, including, say, a dietitian or a mental health counselor, if needed.
“Often doctors don’t know that patients are having trouble with their medications or [aren’t] able to follow a diet plan, and patients are often reluctant to share this information with the doctor or simply are too overwhelmed with their care,” Nundy says. “Caregivers can advocate for their loved ones simply by listening and sharing with the doctor, and then trusting them to make the right decisions that reflect their loved ones’ needs.”
Find Support for Yourself
The best way to be a caregiver is to take care of yourself, too. “Not only does the patient feel stress, but I think it’s important to explain that the caregiver can feel the stress,” says Kathryn Leciejewski, PharmD, BCACP, who works with Strauss and Koustis at the VA. “Acknowledging it can help with coping with it.” If you can find a support group for caregivers, so much the better. Kara Wilson was able to meet other parents of children with diabetes after her son, Isaac, was diagnosed with type 1 diabetes in 2012. “It helps so much to meet others who are going through exactly what you are dealing with,” Wilson says. “We need to hug each other and take comfort in the support we can offer one another.”
B. DIABETES MANAGEMENT – PATIENT SELF-MANAGEMENT AND HEALTH EDUCATION
Health Educators deliver Community-based Lifestyle Change Programs: The CDC DPP Curriculum is based on the Diabetes Prevention Program (DPP). The DPP was a clinical research study led by the National Institutes of Health and supported by the Centers for Disease Control and Prevention. Studies subsequent to the DPP determined how best to implement the program where people live and work. Read more about the curriculum. http://www.cdc.gov/diabetes/prevention/recognition/curriculum.htm
Diabetes self-management is seen as the cornerstone of care for all individuals with diabetes who want to achieve successful health-related outcomes and is considered most effective when delivered by a multidisciplinary team with a comprehensive plan of care. There is a growing body of literature on both educational and psychosocial interventions, aimed at helping individuals to better manage their diabetes. There is some evidence for the effectiveness of self-management education, including community-based peer support groups and ongoing home telephone support.
Online support: http://www.diabetesselfmanagement.com/about/
Community-based peer support: http://moarthritis.typepad.com/northeast_missouri_rac/ - (Living a Healthy Life classes) –
LOCAL: http://moarthritis.typepad.com/northeast_missouri_rac/Kirksville%20DSMP%…
Diabetes Self-Management Toolkit: http://moarthritis.typepad.com/selfmanagement_toolkit/chronic-condition-…
C. DIABETES SELF-MANAGEMENT AND PHYSICAL ACTIVITY
Assessments:
Physical Activity readiness Questionnaire: http://exerciseismedicine.org/documents/A_EIM_PAR-Q.pdf
Health Education: http://diabetes.niddk.nih.gov/dm/pubs/physical_ez/ ; http://www.diabetes.org/food-and-fitness/fitness/
D. DIABETES SELF-MANAGEMENT: MAKING AN ACTION PLAN WITH YOUR CLIENT
My visit with: Dr. Thomas Date: June 15, 2009
Things we talked about / Things I need to do:
http://www.diabetes.org/food-and-fitness/fitness/
Increase evening insulin dose from 20 to 25 units.
Make an appointment with the eye doctor. Call Main Street Ophthalmology at 555-9837.
Action Plan
One goal I want to achieve that will improve my health:
Lose 10 pounds with exercise and diet changes
One specific step I can take to achieve this goal:
Increase my exercise with regular walking.
What: Walking
How Much: 30 to 40 minutes
When: During my weekday lunch breaks; Sunday or Saturday morning in the neighborhood with my wife.
How Often: Four times a week
How sure am I that I can do this?
1 2 3 4 5 6 7 8 9 10
Not sure Very sure
Consultation 2: Smokeless Tobacco Cessation
Health Educators/Health Education Specialists: Job Description
The U.S. Department of Labor Bureau of Labor Statistics (BLS) defines health educators (SOC 21-1091.00) as those who promote, maintain, and improve individual and community health by assisting individuals and communities to adopt healthy behaviors, collect and analyze data to identify community needs prior to planning, implementing, monitoring, and evaluating programs designed to encourage healthy lifestyles, policies and environments. They may also serve as a resource to assist individuals, other professionals, or the community, and may administer fiscal resources for health education programs. http://www.bls.gov/soc/soc_f1j1.htm
Health Education Specialist Responsibilities and Competencies
Area I: Assess Needs, Assets and Capacity for Health Education
Area II: Plan Health Education
Area III: Implement Health Education
Area IV: Conduct Evaluation and Research Related to Health Education
Area V: Administer and Manage Health Education
Area VI: Serve as a Health Education Resource Person
Area VII: Communicate and Advocate for Health and Health Education
Brief Video about Certified Health Education Specialists/Roles and Responsibilities: http://www.sophe.org/healthedspecialist.cfm
Brief Videos: What is Public Health/This is Public Health:
http://www.whatispublichealth.org/what/
http://www.thisispublichealth.org/video_lowres.html
————————————————————————————————————–
A. SMOKELESS TOBACCO AND TOBACCO CESSATION – HEALTH EDUCATION
Mouth lesions - Leukoplakia is a white patch in the mouth that can become cancer. These are sometimes called sores but they are usually painless. Many studies have shown high rates of leukoplakia at the place in the mouth where users place their chew or dip. One study found that nearly 3 out of 4 daily users of moist snuff and chewing tobacco had non-cancerous or pre-cancerous lesions (sores) in the mouth. The longer a person uses oral tobacco, the more likely they are to have leukoplakia. Tobacco can irritate or destroy gum tissue. Many regular smokeless tobacco users have receding gums, gum disease, tooth decay (from the high sugar content in the tobacco), and bone loss around the teeth. The surface of the tooth root may be exposed where gums have shrunken. All this can cause teeth to loosen and fall out.
http://www.cancer.gov/cancertopics/factsheet/Tobacco/smokeless
http://www.cancer.org/cancer/cancercauses/tobaccocancer/smokeless-tobacco
http://www.nlm.nih.gov/medlineplus/smokelesstobacco.html
Quitting resources:
http://www.nidcr.nih.gov/oralhealth/Topics/SmokelessTobacco/SmokelessTobaccoAGuideforQuitting.htm
Consultation 3: Discharge Planning
Health Educator/Health Education Specialist NOTES and ASSESSMENTS
Health Educators/Health Education Specialists: Job Description
The U.S. Department of Labor Bureau of Labor Statistics (BLS) defines health educators (SOC 21-1091.00) as those who promote, maintain, and improve individual and community health by assisting individuals and communities to adopt healthy behaviors, collect and analyze data to identify community needs prior to planning, implementing, monitoring, and evaluating programs designed to encourage healthy lifestyles, policies and environments. They may also serve as a resource to assist individuals, other professionals, or the community, and may administer fiscal resources for health education programs. http://www.bls.gov/soc/soc_f1j1.htm
Health Education Specialist Responsibilities and Competencies
Area I: Assess Needs, Assets and Capacity for Health Education
Area II: Plan Health Education
Area III: Implement Health Education
Area IV: Conduct Evaluation and Research Related to Health Education
Area V: Administer and Manage Health Education
Area VI: Serve as a Health Education Resource Person
Area VII: Communicate and Advocate for Health and Health Education
Brief Video about Certified Health Education Specialists/Roles and Responsibilities: http://www.sophe.org/healthedspecialist.cfm
Brief Videos: What is Public Health/This is Public Health:
http://www.whatispublichealth.org/what/
http://www.thisispublichealth.org/video_lowres.html
If Transition to Rehab:
Certified Health Education Specialist (CHES) “Consult” - Health Education/Community and Public Health:
“As a health care professional, you assess patients all the time. But you generally do not assess a patient’s family caregiver, except to identify that person as a “resource” or “informal support” when developing a discharge plan. In this traditional view, the family caregiver, who is not a client or a beneficiary and not an official part of the health care team, is typically outside the realm of professional responsibility. Like so much of health care today, that view is changing. Increasingly professionals “hand off” very sick or disabled patients to family caregivers after a hospital stay, a short-term nursing home stay, or an episode of home care services. In these transitions, especially when the patient is elderly or chronically ill, the patients’ continued health and well-being depends on a family caregiver. That person must be willing and able to handle the patient’s complex health, financial, legal, and social needs. Sometimes these tasks are temporary, while the patient recovers; in the case of elderly or seriously ill patients, the job can continue for months or years.
Caregiver assessment is a tool to help identify strengths and limitations to help develop a realistic plan for the next stage of care. The goal is twofold: (1) to ensure that the patient’s health and well-being are maintained and enhanced; and (2) to ensure that the caregiver’s capacities and needs are considered and addressed in a care plan.”
Health Educators conduct “assessments”; so….
“I would recommend…” …A Caregiver’s Assessment: ask John about…
- The caregiver’s background, including age, education, employment, other family responsibilities, living arrangements.
- The caregiver’s perception of the care recipient’s health and functional status.
- Length of time the caregiver has been providing care; if is a new event, what the caregiver worries most about in providing care.
- Values and preferences about caregiving (“do it all myself,”; “can’t deal with needles or incontinence,”; “I can’t take Mom to my home because there just isn’t room for another person”).
- Caregiver’s health status, including any limitations relevant to caregiving.
- Impact of caregiving on emotional status, finances, other family members.
- Knowledge, skills, and abilities to perform necessary caregiving tasks.
- Resources used or interested in accessing.
In introducing the assessment process to the family caregiver, the assessor should clarify the goals of the assessment and make it clear that all information (unless specified by the caregiver) will be shared with the health care team in order to develop a care plan. The assessor should also summarize the conversation, so that the family caregiver feels that his or her concerns have been heard. The assessor can emphasize the positives first, and then list the areas where some questions have been raised, and suggest a process for following up.
If Transition from Hospital to Rehab-
Certified Health Education Specialist (CHES) “Consult” - Health Education/Community and Public Health:
“Health Educators plan and implement evidence-based programs/interventions, so I would recommend some resources….”
Patient Education: Diabetes self-management is seen as the cornerstone of care for all individuals with diabetes who want to achieve successful health-related outcomes and is considered most effective when delivered by a multidisciplinary team with a comprehensive plan of care. There is a growing body of literature on both educational and psychosocial interventions, aimed at helping individuals to better manage their diabetes. There is some evidence for the effectiveness of self-management education, including community-based peer support groups and ongoing home telephone support.
Online support: http://www.diabetesselfmanagement.com/about/
Community-based peer support: http://moarthritis.typepad.com/northeast_missouri_rac/ - (Living a Healthy Life classes) –
LOCAL: http://moarthritis.typepad.com/northeast_missouri_rac/Kirksville%20DSMP%…
Diabetes Self-Management Toolkit: http://moarthritis.typepad.com/selfmanagement_toolkit/chronic-condition-…
Public Health Management of Diabetes/Evidence-based Interventions:
http://health.mo.gov/data/interventionmica/Diabetes/index_5.html
The research/evidence behind community-based exercise/nutrition interventions for chronic disease: http://academiccommons.columbia.edu/catalog/ac:156754
We recommend the Community Guide as a starting point to finding best-practice interventions for nutrition/exercise programs in your community: http://www.thecommunityguide.org/index.html
In Missouri: MICA: http://health.mo.gov/data/interventionmica/
Physician & PA
Admit H&P
Age: 80M
HPI: This 80 yo male widower from Edina, MO, presents to Blessing Hospital with c/o feeling fatigued. This T2DM patient taking insulin noticed a sore on his Right great toe 3 weeks ago. Treated x 1 week by home health nursing and antibiotics. Admits poor compliance with antibiotics. Treated primarily with soaks. Saw PCP in Edina who sent patient to BH for admit.
PMH:
Illnesses: T2DM x 6 mos
Injuries: Injured his back lifting hay bales in 1990
Hospitalizations: Back surgery 1990, Croup as a child (c.1940)
Surgeries: L4-L5 laminectomy c. 1990, TURP- c.2008
Medications:
- Metformin 1000 mg PO BID
- Insulin Lantus 10 Units SQ QD x 1 month
- Benadryl 25-50 mg at HS prn insomnia
- APAP 1000mg prn
Allergies: NKDA
Prevention:
- Diet “anything I want” at home
- Colonoscopy 5 years ago was “fine”
- UTD on pneumovax, TD and gets annual flu shot
- DRE with OB annually
Personal/Social History:
Occupation: retired farmer, served in armed services
Marital Status: Widower x 10 years after married 50 yrs
Support: Lives alone, son and daughter-in-law help with farm chores
ETOH: “couple of beers” (3-4) each night
Tobacco: never smoked. Does chew tobacco.
Illicit drugs: denies
Family History: Son, “Jon”, age 53- alive and well, Grandkids: several A&W
Review of Systems:
Constitutional: + insomnia described as trouble getting to sleep- onset 4-5 months ago. Denies fatigue, weight loss/gain, fever, chills, night sweats.
Eyes: +bifocals to read. Denies vision change, pain, redness.
ENT: Denies headache, hoarseness, sore throat, epistaxis, sinus symptoms, hearing loss, tinnitus. Has noticed “lump” under right jaw.
Skin: Denies rash, pruritis.
CV: Denies chest pain, edema, PND, orthopnea, palpitations, claudication.
Pulm: Denies cough, SOB, wheezing, hypersomnolence.
Breast: Denies pain, mass, discharge.
Endocrine: Denies polyuria, polydipsia, polyphagia, heat/cold intolerance.
GI: Denies Abd pain, stool changes, N/V, diarrhea, constipation, heartburn, blood in stool, melena.
GU: Denies Dysuria, frequency, hematuria, discharge, menstrual probs.
MSK: Denies arthralgia, arthritis, joint swelling, myalgias, back pain.
Neuro: Denies weakness, seizures, peraesthesias, tremor, syncope, + Falls x 2 in past several months, memory loss.
Psych: Denies anxiety, depression, hallucinations, +”feels sad” when he thinks of wife.
Heme/Lymph: Denies bleeding, bruising, clotting, transfusions, lymph node swelling
Allergy/Immunology: Denies hayfever, insect allergies, environmental allergies.
Physical Exam:
- BP: 126/74
- P: 84 regular
- R: 14 unlabored
- T: 99.7
- O2Sat: 98% on RA
General: A&Ox3, cooperative and pleasant affect,
HEENT:
Eyes: PERRL, EOMI, Fundi without lesions, AV-nicking, normal disc; sclerae anicteric; conjunctivae pink
Ears: nl EACs with mild cerumen bilaterally, TMs pearly grey with normal mobility
Nose: nares patent, nasal mucosa pink, no d/c
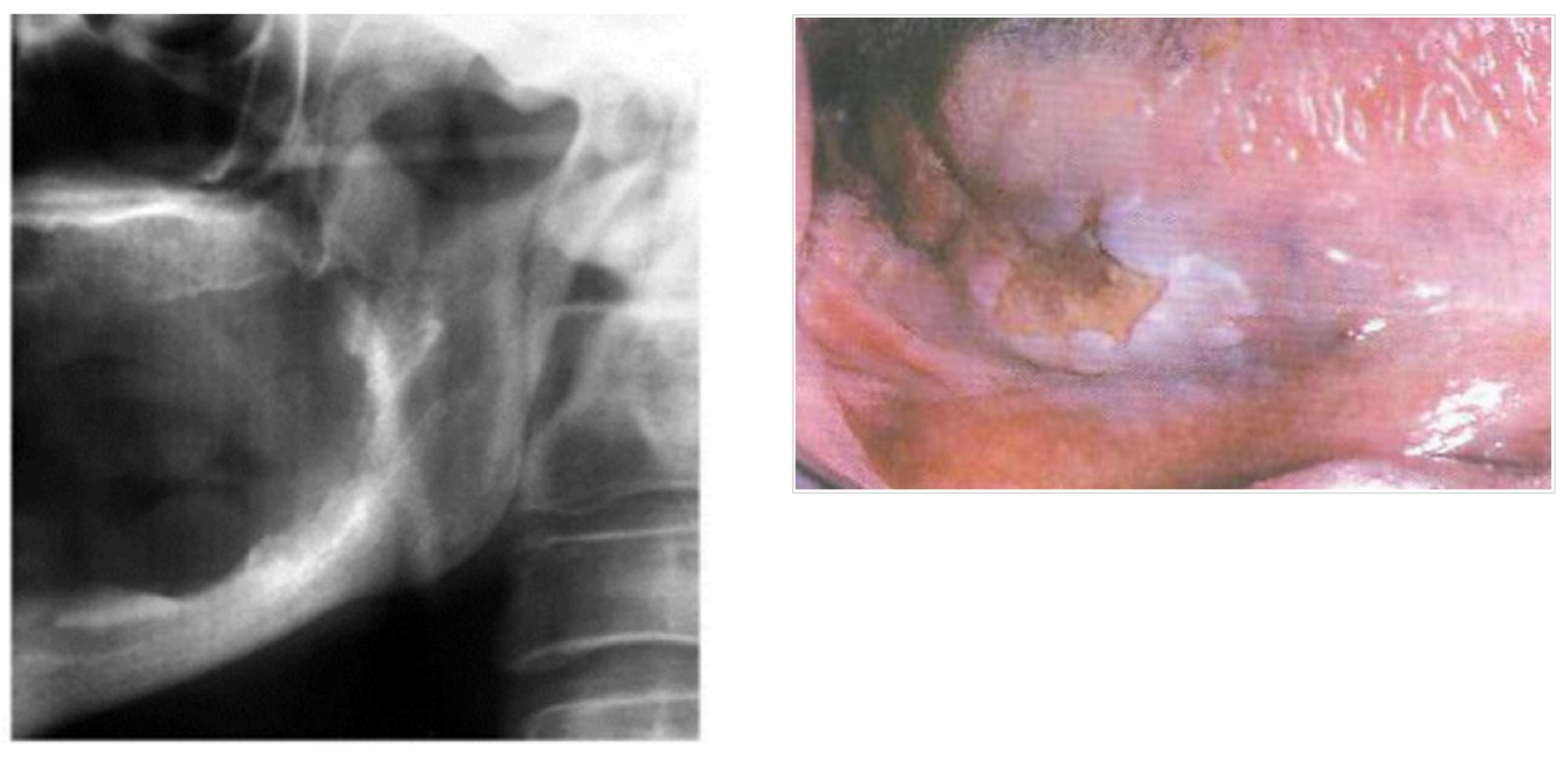
Mouth: with pink moist mucosa, 1 cm lesion rt side of tongue, pharynx non-erythematous
Neck: supple, POSITIVE right submandibular lymphad- mobile, NT mass 1-2 cm in size, no bruits, thyroid symmetrical without enlargement or tenderness
CV: RRR without MRG. Peripheral pulses 2+ and equal bilat in upper and lower exts; normal hair distribution on calves; no bruits
Pulm: Lungs CTAB without adventitious sounds
Abd: Soft and NT without HSM; No scars or lesions
Exts: no clubbing, cyanosis or edema, full NT ROM all exits. 10 gm monofilament 0/10 bilaterally. Vibratory sense intact bilat feet
Skin: 1x 2 cm wound medial rt grt toe, mild erythema, mild exudate,
GU/Rectal: Perianal external normal, Normal tone, formed brown stool neg for OB. Uncircumcised male with no lesions or d/c; Testicles symmetric, NT, no masses.
Neuro: CN II-XII grossly intact. Full equal strength and sensation bilaterally. Romberg negative. DTRs 2+ and eq bilaterally
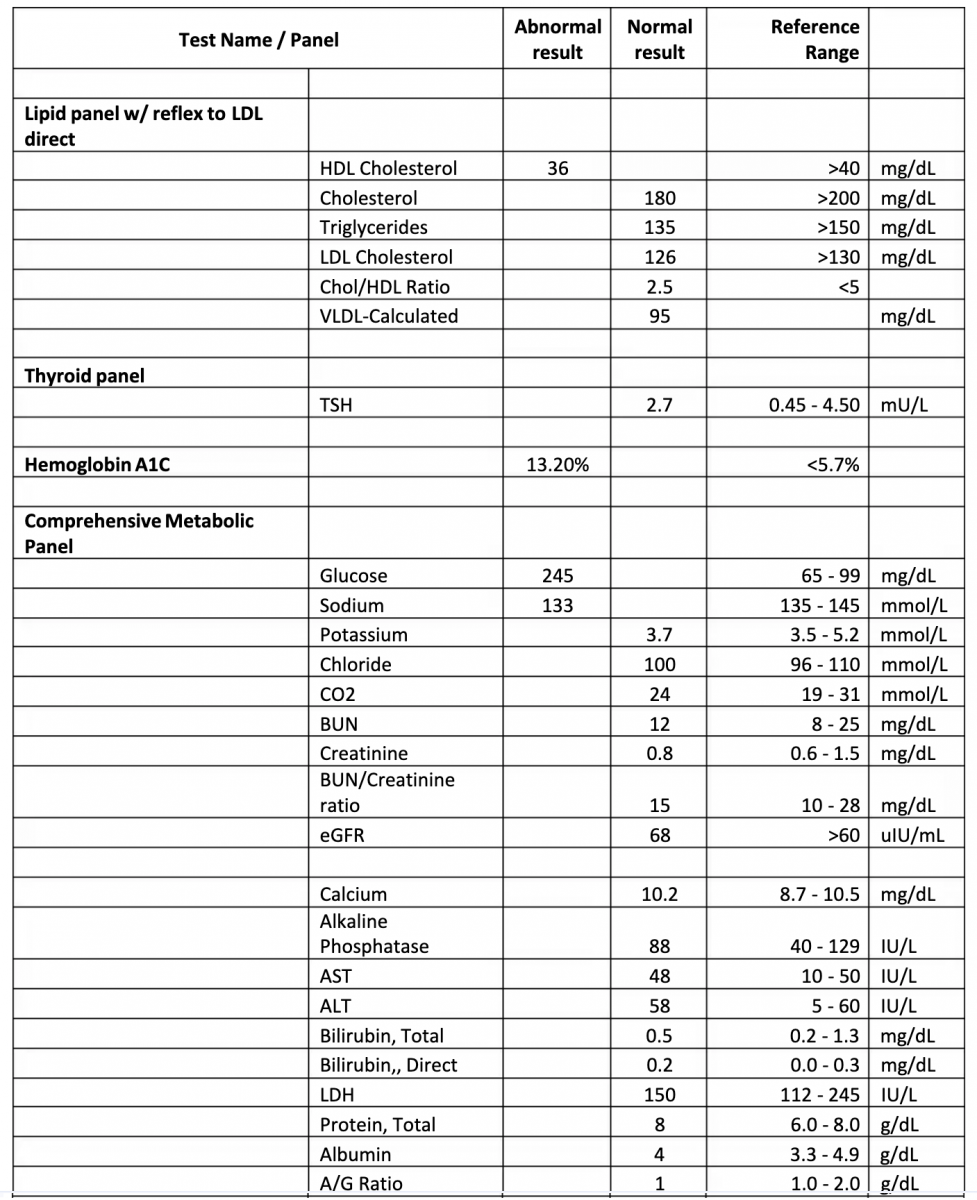
Labs
- Diabetic foot ulcer
- T2DM
- Sepsis
Plan:
- Admit to Medicine
- Diagnosis: 1)Diabetic foot ulcer, 2) T2DM, 3) Possible Sepsis
- Condition: Fair
- Code status: Full
- Allergies: NKDA
- VS q Shift
- Activity: OOB ad lib
- Nursing: wound care right great toe BID. Accuchecks AC and HS
- Diet: 1800 calorie ADA
- IV: 0.9% NS to KVO
- Meds: Zosyn 4.5 gm IV q6hr (start after blood cultures drawn). Vancomycin 1 gm IV q 12 hr. Fingerstick BGs AC and HS with sliding scale insulin Lispro: Goal Blood Glucose is <150. BG 150-199: 1 unit bolus Insulin Regular. BG 200-249: 2 units bolus Insulin Regular. BG 250-299: 3 units bolus Insulin Regular. BG 300-349: 4 units bolus Insulin Regular. BG Over 350: 5 units bolus Insulin Regular. MOM 30 cc po prn constipation. APAP 650 mg po q 6hr prn maild pain or fever. Ambien 10 mg PO @ hs prn insomnia
- Labs: Blood cultures x 2 sites now. CBC, BMP q AM
- Consult PT re: wound care
Bob Jones, PA-C
Physical Therapy
Reason For This Admission: Open wound R great toe, Sepsis, Type II DM
PMHx: L4-L5 Laminectomy (1990, approx.); TURP (2008, approx.)
Physical Therapy Initial Evaluation
O: History: Patient diagnosed with DM 6 months ago and began using insulin 1 month ago. Patient developed a wound on the right great toe 3 weeks ago and was being seen by home health nursing. Wound regressed and patient admitted to hospital with sepsis.
Social: Patient lives alone in a farm house. Patient cooks all meals and obtains fresh eggs from chicken coop every morning. Son and daughter-in-law live close by and assist patient when needed, including caring for farm animals. Patient visits with friends 1x/week at VFW. Patient ambulates without an assistive device. Patient reports he quickly gets tired when walking. Patient reports falling twice in past month when he “got up too quickly”.
Cognition: A & O x 3. Follows directions throughout session.
Sensation: Patient unable to feel the 1gm and10gm monofilaments but can feel the 75gm monofilament on bilateral feet.
Motor: AROM bilateral LE: WNL. Strength: grossly 3/5.
Balance: One-legged stance test with eyes open is 10 seconds and with eyes closed is 2 seconds.
Mobility: Bed mobility: Independent. Patient complained of mild dizziness when transitioning from sit to stand, dizziness resolving quickly. Ambulated with a slow gait pattern 75 feet using front wheel walker. Moderate assist required to help patient maintain non-weight bearing on ulcer. Two standing rests needed due to fatigue. No loss of balance when walking. Patient had difficulty limiting weight bearing through ulcer. Stairs/steps not assessed. Patient tolerated sitting in chair x 30 minutes.
Wound: Located on medial right great toe. Wound measures 1.0cm x 1.5cm and surface area is 1.5cm2. Wound edges are callused. Wound bed is 50% yellow necrosis and 50% pale pink viable tissue. Minimum exudate. Erythema noted around peri-wound.
A: Major impairments and activity limitations include:
1. No protective sensation bilateral feet
2. Neuropathic ulcer on weight-bearing surface
3. LE weakness
4. Impaired balance
5. Reduced gait speed
6. Difficulty not placing weight through ulcer with ambulation
7. Limited endurance
8. Moderate assistance for walking indoors on level surfaces (assistance primarily needed to decrease weight bearing through ulcer)
Goals:
1. Ambulate 150 feet with 0-1 standing rest breaks using front wheel walker and off-loading shoe on level surface.
2. Tolerate sitting in bedside chair for at least 1 hour.
3. Increased LE strength by ½ grade to 3+/5 for increased use in ADLs.
4. No complaints of dizziness when transitioning from sit to stand.
5. One-legged stance test will improve to 14 seconds with eyes open to decrease risk for falls.
P: Therapeutic exercise and mobility training QD-BID x 3-5 days. Progress sitting tolerance and distance walked. Patient and family education. Discharge planning. Patient would benefit from an offloading shoe to enable patient to ambulate while also offloading ulcer for wound healing. Order needed equipment (e.g. FWW; off-loading shoe)
Claudia Sutton, PT
Progress Note, Next Day
S: “I’m glad you are here. I want to get moving so I can get stronger and get out of this place.” At end of session, patient asked about getting a walker for home. “I feel more steady with it.”
O: Patient went from supine to sitting edge of bed independently. Patient shown how to don new offloading shoe. Patient was educated on the importance of wearing the shoe to relieve pressure so the wound so it can heal. Patient transitioned from sit to stand independently. Worked on standing balance activities while wearing off-loading shoe. One-legged stance test with eyes open was 12 seconds. Patient slowly ambulated 100 feet using front wheel walker and offloading shoe. One standing rest needed due to fatigue. No loss of balance noted. Patient performed seated lower extremity strengthening exercises, including glut sets, quad sets, hip flexion, knee extension, and ankle pumps, 10x/set, 1 set each. After treatment, patient tolerated sitting up in chair for lunch x 45 minutes.
A: Patient did well with new offloading shoe. Patient was able to ambulate without weight-bearing through ulcer. Gait was steady and patient reports feeling more steady using walker. Endurance improved as patient was able to ambulate further, take fewer rests, sit in chair longer, and perform more activities (balance and exercises). One-legged balance also improved, but is still not WNL.
P: Continue gait training, balance activities, and strengthening exercises QD-BID. Patient will need front-wheel walker ordered.
Claudia Sutton, PT
Social Work
Biopsychosocial Assessment
Patient Name: Sherman “Red” Yoder
Age: 80 yrs
Presenting problem: Patient is being referred to social services for assessment of family dynamics between the patient and his son. The patient and son reportedly had an argument in the presence of the occupational therapist during which the son shouted “I just can’t possibly do anymore!” The patient reportedly relies on his son to meet all of his needs including assisting him manage the family farm.
Personal History/Family History: The patient is an 80 year old man who lives in the same farmhouse that he has lived in all of his life. He was married to his childhood sweetheart, Bessie for 50 years. He states they had a very good life together. Bessie passed away 10 years ago. The patient has one son, Jon age 53, who he relies on quite a bit. He notes that Jon has been very impatient and agitated with him lately and that he is “scared” of his son. He states that Jon “got real mad” during a recent trip to the mall. The patient reports that he and Jon have always had a “difficult time getting along” but that things have become “real bad lately.” “I guess Jon never forgave me for not being there for him when he was growing up. I always had so much to do and never really paid all that much attention to him.” The patient denies any abuse by his son and clarifies “I’m scared to speak up.” The patient states that the farm “means the world to him” and that “moving away would be the end” of him. He adds that he wants to “will” the farm to his grandson since Jon “never really had an interest.” He states that he just “wishes Jon would understand” and stop pushing him to sell the farm.
Vocational/Military History: The patient retired from work at the age of 65 years old. The patient reports he served in the Korean War for the Army for a brief time. Upon his return home, the patient managed his farm full time. He served in the Army long enough to receive Veteran’s benefits and gets Social Security retirement benefits. These are his only sources of income.
Medical History: Patient reports he has “sugar diabetes” and that he cannot understand why he is sick as he thinks he is “doing just fine.” He states he “took pills for it” but has recently been “given insulin.” He reports he takes his medications but sometimes skips a dose when his “blood sugar is high without eating.” He adds that he sometimes “just plain forgets” to eat. He describes his diet by saying, “I eat whatever I want. I sometimes forget whether or not I have eaten and so I eat again just to be sure. I don’t want my blood sugar to get low.” When asked about how he prepares food, the patients states, “I just eat whatever I can get my hands on. You know, easy stuff like noodle soup, bread, beans. I was never one for cooking, Bessie always did that, Lord rest her soul. I sure miss her.” The patient also reports difficulty with sleeping and that he takes Benedryl to help “slow down.” He adds that getting up in the morning is difficult as he feels “stiff.”
Mental Health/Substance Abuse History: The patient denies any history of mental illness but reports he “sure feels sad” when he thinks of Bessie. He describes feeling “lonely” without her and that he is just “beside” himself. He adds how Bessie did all the “inside work” and how he “just don’t know what to do.” The patient starts to cry but recovers quickly. In relationship to use of substances, he reports that he “drinks a couple of beers” at night to help him sleep. When asked how many is meant by “a couple” he states that he usually drinks 3 to 4 beers a night. He reports he started drinking beer at night 3 to 4 months ago. When asked whether or not he gets intoxicated, he states, “drunkenness is a sin.” He did say that his son Jon “gets after” him about his drinking but that he “pays him no mind.”
Social Support System: The patient states that he relies solely on his son and daughter in law to help him meet his daily and weekly needs. He states that his son cares for the farm i.e. feeding the animals and taking care of the crops while his daughter in law, Judy helps him with doctor appointments, going to the grocery and picking up his medicines. The patient states that it must be hard on his son as he is an only child. He adds that from time to time the ladies at the church offer to help out but he does not want to “be a burden to them.” He states that he enjoys visiting with them at church every week and they were “real nice” when Bessie died, but that “it just ain’t right” to ask for their help. The patient also reports having good relationships with his grandchildren and that he loves them very much. He adds that he really looks forward to his weekly skype sessions with his grandson in college.
Leisure: The patient states that he “goes into town” each week to the VFW and visits with other Veteran’s. He notes that this is one of the few places that he can drive to without “getting lost.” The patient makes reference to his doctor moving into a new office and how difficult it is for him to find his way. He adds that this is the reason why Judy now drives him to his doctor appointments. Other things he likes to do include gathering eggs each day and making breakfast. He states, “I always was the one who made breakfast in the morning. Thank God I haven’t forgotten how to do that!” Other leisure activities include church functions, spending time with his grandchildren, and “surfing the web.” The patient notes that he started to use computers as a way to manage inventory and noticed it was “real fun.”
Self-Care: The patient reports he is “doing just fine.” He describes his daily routine to include getting up, gathering eggs, making breakfast, surfing the web, and drinking a couple of beers at night. The patient reports that he sometimes forgets to take his medications and that he also loses track of time and “forgets to eat.” The patient states he prepares “simple meals” because he is “not much of a cook.” He manages to “get around town” but reports he is often late to where he is going because he “gets lost.”
Assessment: The patient presents as very friendly and agreeable. His support system appears expansive and intact. His son and daughter in law are his sole sources of support as of now. Another source of support could be his church and friends from the VFW. The patient also has enough leisure activities to occupy his time and make life rewarding. There are several areas of concern that need to be addressed. First, the patient’s residence is too much for him to manage on his own. He must rely on outside sources of support to manage the workload involved in having a farm. Second, the relationship between the patient and his son is currently strained and appears to have always been characterized by continuous strife. This is worsened by the patient’s unwillingness to engage other sources of support to assist him at the current time. Furthermore, the patient’s son appears to be experiencing caregiver fatigue and any service planning should include alleviating the son’s level of responsibilities and psychosocial stress. Third, the patient appears to have a poor understanding of diabetes and the progression of the disease process. He also appears to have little understanding of the consequences of his diet and not taking his medications the way they are prescribed. He seems to be unwilling to comply with dietary restrictions stating “I eat whatever I want.” It is possible that this is the result of inadequate life skills as the patient did rely on his wife to do the cooking. Additionally, it is not uncommon for men in his age group to not know how to cook. The patient may need to be taught a few basic skills in order to improve his eating habits. Fourth, the patient appears to have some level of cognitive deficit as evidenced by forgetfulness, getting lost, and decline in self-care abilities.
Plan: In order to increase biopsychosocial stability the following will be addressed:
- Further explore support-system and determine if farm-related tasks and errands can be delegated to church friends or friends from the VFW.
- Refer to Area Agency on Aging programs for diabetic diet home delivered meals and assistance with housekeeping/independent living.
- Refer patient’s son to a caregiver support group.
- Request a consultation for diabetes education.
- Further explore reasons for “forgetting” to take medications and problem-solve solutions. Refer to nursing if needed.
- Request evaluation of cognitive deficits to rule out dementia.
- Provide information about long term care program for future use.
Celia Spadafino, MSW
Speech & Language Pathology
Initial Evaluation
Reason For This Admission: Open wound R great toe, Sepsis, IDDM
Reason For Referral: Pt is not meeting nutritional needs complicating diabetic status.
PMH: L4-L5 Laminectomy aprox 1990, Prostate surgery/TURP , approx 2008
S: “It’s my toe, not my mouth.” when the therapist introduced herself as a speech/language pathologist. He was ask if he was having trouble eating and he responded “Oh yeah, that. - O.K.” The Pt was referred by physician and dentist who indicated the Pt was not meeting nutritional needs and nursing suspected the Pt has painful chewing. It was noted that social work indicated some possible cognitive and OT indicated the MOCA score suggested mild cognitive impairment.
O: Client’s chart was reviewed and discussed with nursing Pt’s PO intake. A bedside dysphagia eval was completed.
Oral/peripheral exam findings were as follows: All oral/motor structures were WNL for symmetry, ROM, tone, strength, and coordination. The Pt’s teeth are adequate for mastication. His soft and hard palate have a normal appearance. It was noted that there was a significant lesion on the right lateral tongue with some extension into the R lingual alveolar sulcus. His voice was WNL for his age and gender and he was able to vary his pitch and loudness readily suggesting adequate airway protection.
Clinical Bedside Swallowing Assessment Findings:
Observations: The Pt was A & O and able to self-feed. He was cooperative and followed directives throughout the session.
Reports by Patient, Family and Staff: Nursing reports that the Pt is not meeting his nutritional or hydration needs in order to maintain his healthy glucose levels. He is consuming less than half of his meal trays. The Pt’s daughter-in-law was present during the eval and indicated that she had not noticed any issues with his eating, but she was not always with him during meal times.
Examination by the Pt’s physician and then by a dentist indicated the Pt had a lesion on the R-lateral side of his tongue. When ask why he was having trouble eating the Pt denied pain at first, but then admitted to having pain when consuming food or liquid.
Nourishment Intake Status: The Pt is currently on a regular texture diabetic diet with thin liquids. At home the Pt reports that he eats “whatever” he wants that is available and easy to fix.
PO Trials:
- The Pt was able to take a drink of thin liquids from a cup w/o labial loss. His swallow response time was WNL, but there was an audible gulp.
- He was able to form a bolus with puree texture but utilized an open-mouth posture. Swallow response time was WNL.
- With solid textures the Pt again utilized an open-mouth posture and took a significant amount of time to masticate the bolus and move it posteriorly. It was noted there was residue in the alveolar sulcus suggesting difficulty forming a cohesive bolus. The swallow response time was WNL.
A: The Pt is demonstration an oral phase dysphagia as indicated by uncoordinated bolus formation and residue in the oral cavity after the swallow response had occurred. Difficulty is probably due to painful mastication as a result of the observed lesion. There is a risk of aspiration after the swallow response due to residuals in oral cavity. There are no clinical signs of aspiration at this time (temperature spikes, “wet” lung sounds).
P:
- Complete the St Louis University Mental Status Exam (SLUMS) to determine if the Pt will be able to follow directives on safe swallowing.
- Recommend a Videofluoroscopic Swallowing Study (VFSS) to establish a baseline and R/O aspiration.
- Provide the Pt and his caregivers with a list of strategies for safe and less painful swallow (see below).
- Recommend that the Pt be placed on a soft texture diet.
- Continue to monitor for changes in status of the oral cavity.
Recommended swallow strategies to decrease painful episodes:
- tilt head to the left in order to direct material away from lesion site.
- after each bite take a sip of thin liquid to clear oral cavity.
- avoid salty and spicy foods
- adhere to diabetic diet
Ida Best CCC/SLP
SPEECH/LANGUAGE PATHOLOGY Progress Note
S: Pt seen in his room while sitting in the chair for screening of cognitive/memory status. This therapist was informed by nursing that due to eminent DC they were unable to schedule a VFSS in radiology.
O: The SLUMS was administered. The Pt scored 25 out of 30. Results of the screening were explained to the client and recommendations were given and provided in writing.
A: Scoring reflects a potential mild cognitive deficit with the Pt showing the most difficulty with delayed recall of the 5 objects listed and difficulty holding information in mind in order to process a simple math problem. The Pt is able to understand directives, but will require assistance of memory strategies and caregiver support in order to follow through with recommendations. bThe Pt agreed with the findings and stated he is willing to follow through with recommendations.
P: Recommendations:
- As indicated in previous SLP note regarding PO intake and positioning.
- Complete outpatient VFSS.
- Obtain physician’s order for SLP re-eval if difficulty with mastication gets worse.
- Maintain written lists to assist with memory recall of items of importance (positioning strategies, diet recommendations, grocery lists, ADL that need to be completed etc).
- Maintain a calendar of events in order not to miss medical appts.
Ida Best CCC/SLP
Dental
Comprehensive Dental Exam
S: Mr. Red is a 80 yo Caucasian man who was admitted to the hospital three days ago because of open wound on his right toe and sepsis due to type II diabetes.
CC: “Sore in the mouth but, I have no teeth to for the dentist to see me!”
Med HX: L4-L5 Laminectomy aprox 1990, Prostate surgery/TURP, aprox 2008
Patient was diagnosed with DM six months ago and is on insulin since one month ago. Patient developed a wound on the right great toe 3 weeks ago and was being seen by home health nursing. Wound regressed and patient admitted to hospital with sepsis.
Allergies: NKDA
Medication HX:- Metformin 1000 mg PO BID
Insulin Lantus 10 Units SQ QD x 1 month
Benadryl 25-50 mg at HS prn insomnia
APAP 1000mg prn
Zosyn 4.5 gm IV q6hr (start after blood cultures drawn)
Vancomycin 1 gm IV q 12 hr
Social Hx: Patient is a widower, lives alone in a farm house with his son living nearby.
Chewed tobacco since he was a teenager.
Alcohol use, a social drinker
Denies weight loss but has lost 20 pounds since last year.
Dental Hx: Pt has been wearing U/L denture for the past approx. 30-35 years.
Ill-fitting denture, but no complain.
Sore tongue
Pt doesn’t understand why he is being visited by the dentist since he has no teeth in his mouth!
O: BP: 133/91 mmHg P: 69 bpm
Blood sugar: 145 mg/dL
Clinical Exam:
EOE: raised, firm nodule on L temporal region near hairline 10mmx6mm, L forehead 1/2 inch x 1/2 inch
Scar from hx of basal cell carcinoma (not mentioned during medical Hx review)
Rubbery- hard R submandibular lymphadenopathy with pain
IOE: Redness around the corner of the mouth.
Red and white and mixed irregular patch, 1 cm lesion with central ulceration with indurated border on the R lateral border of the tongue.
TMJ: R pop upon opening
OSC: immediate referral to OS
Hard Tissue: Pt has full upper/lower denture
X- Ray reveals irregular outline radiolucency of R anterior border of mandibular ramus with corticated border
A: Candidiasis / Angular cheilitis
Perio Dx: N/A
Caries risk: N/A
OC risk: high due to tobacco use
Athletic Trainer
coming soon
