Gila Hospital Outpatient Department, Tubac Community Health Center, and Dental Clinic
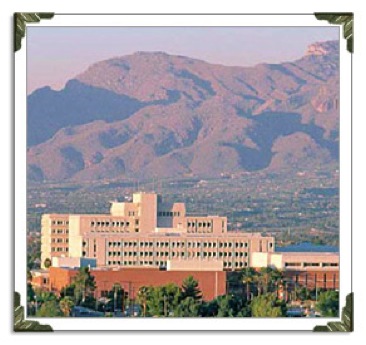
Located in the heart of Tucson, Arizona, Gila Hospital is a 500-bed, not-for-profit hospital that provides a wide range of health, social and support services. Gila Hospital is a nationally recognized center for quality tertiary care, medical education and research. It is a Level I Trauma Center verified by the American College of Surgeons and is also a respected center for maternity care, orthopedics, oncology and many other medical services. Gila Hospital offers both inpatient and outpatient services.
Outpatient Services
Outpatient rehabilitation services are available for individuals with orthopedic, neurological, cardiopulmonary, or other conditions requiring concentrated therapy for return to a maximum level of function for school, work, home management and leisure/recreational pursuits. Outpatient rehabilitation emphasizes patient and family participation in the therapy process to foster the patient’s independence upon discharge. It is our goal to see patients live successfully without our help.
The clinical staff of experienced professionals includes Physical Therapists, Occupational Therapists, Speech-Language Pathologists, Social Workers, and Certified Rehabilitation Nurses. Prior to the start of treatment, authorization from the patient’s insurance company must be received. The length of treatment and frequency of visits are based on several factors including specific injury/condition, the physician recommendations, surgeon or case manager’s prescription, therapist’s evaluation and recommended treatment plan, and insurance coverage.
Gila Hospital outpatient rehabilitation also has evaluation clinics that include specialized services and/or physician/dental consults in the areas of Audiology and Dentistry.
Outpatient Services - Other
Community Health Center - Primary Care Physician, DO
Dental Services
Case Notes
Occupational Therapy
Occupational Therapy Assessment
Gila Hospital, Outpatient
Date of Assessment: 9/17/11
S: “It feels good to get away from the house for a bit. Wow….that homebound status thing is kind of strict. It makes you feel like a prisoner in your own home. I thought I was going to lose it.”
O: OTR/L began eval. Pt is a 38 yr old married man from Tubac who was injured by an IED while in Afghanistan while working as a photojournalist. He sustained multiple wounds to the L side of his body and a L side skull fx. Since then he has experienced some R sided visual neglect, difficulty with visual scanning, R hand edema that seems to have resolved now, executive function problems, difficulty with eating probably due to mouth pain due to multiple injuries and tooth extractions. He developed infection at the L femur pin sites of the external fixator used to repair multiple fx there. He is now WBAT. Has hx of MRSA. Wife reports that he is easily agitated, possibly depressed, and does not seem to have interest in things that he pursued previously. She reports he is fixated on the idea that he should be able to drive even though he has a seizure disorder and R upper visual field cut. She reports he is frustrated with clumsiness and short tempered with the kids. Wife reports that he knocks things over a lot while he is eating or at the bathroom sink, and when he does, he sometimes falls into a rage or becomes very sullen and starts rehashing all that has happened to him and wondering if they would all be better off without him. She admits there is much financial strain but his parents and her parents have helped to make the house payment and friends from her church have frequently filled up the car with gas at their own expense. She feels grateful for the help, but he is mostly embarrassed that they need assistance, and feels guilty that he is not working.
OT EVAL Today Reveals:
Strength: UE WNL, perhaps slightly weaker on the R hand.
ROM: WNL all joints of both UEs
Endurance: Low, frequently sleeps till noon on days he did not have home health, refusing to join family functions
Cognition: Wife reports she must verbally prompt him to shower and dress even though he can physically do it. She reports that he uses his I phone to keep track of apts. She fills medicet and his phone is programmed to remind him of meds, but he still misses his Dilantin aprox 1x a week. Last seizure was aprox 1 month ago. Wife believes he may have had others that he has failed to report to her and she believes he does this because he wants to drive.
Bathing: with SBA and verbal prompts, using tub transfer bench and grab bars. Uses shower pick to mouth.
Dressing: I UE and LE
Grooming: Wife says pt grew a beard that she hates because he did not want to shave anymore. She says he often missed patches of growth on the R side of his face even when he did shave.
Mouth Care: pt uses shower pick when reminded. Pt has electric toothbrush but says it bothers him and hurts his teeth. Wife complains he has bad breath.
IADL- Currently unable to drive due to seizures and R field cut. Would benefit from OT driving eval and so OTR will phone physician to request.
Shopping, pt tolerates 1 hour in grocery store and can retrieve about 20 items in 1 hour following a list and using grocery cart for support. Pt has difficulty scanning the shelves and finding the items and sometimes makes mistakes such as buying diet when he wants regular, or low fat when he wants regular. He had 1 seizure at the store and now refuses to go back there as he says it is too embarrassing since he became incontinent.
Financial: pt prefers that the wife handle that now even though he tracked their investments and used to insist that they live on a budget that he developed prior to his injury.
Spiritual: Pt states he does not have a religion and wishes his wife would stop trying to get him to go to church or leave him with people who try to convert him into a believer. He does admit he is curious about what happens to a person when they die. He says he feels enlightened when surrounded by nature and hopes to take a family camping trip soon and show the kids things about the stars and rock formations.
Leisure: Pt has interest in photography, music, camping, guitar, reading to the kids, and possibly starting a garden. He is hoping to start going to a gym now that he is not on home bound status.
Sexual: Pt and wife say they do not wish to discuss this issue at this time.
Work: Pt doubts that he will ever be able to work full time as a photographer. He continues to use his IPHONE to take basic pictures, but says he cannot get the shots to line up right when he attempts to use his old professional equipment.
A: Pt has made significant progress from a physical standpoint but now needs interventions to increase endurance, self initiated and organized attention to self care, parenting roles, leisure, and a plan to pursue working if possible. Pt has signs of possible depression as evidenced by agitation, impaired sleep patterns, feelings of low self worth. It is unclear how often he is having seizures and that must be determined if he is to pursue getting a driver’s license. OTR has advised him that he is required to self report his seizure activity to MVD and is not to drive until cleared by his physician and the MVD…typically after at least 3 months of being seizure free.
P:
OT x 3 wks
OT Goals:
1. Increase endurance to at least 12-16 hours out of bed, involved in activity time per day to simulate normal workday.
2. Increase consistent compliance with seizure meds and determine actual frequency of seizures via use of www. myseizuretracker.com or other app.
3. Increase consistent mouth care after consult with dentist for specific recommendations.
4. Increase self-initiated showering. Wife to withdraw verbal prompts and determine if he continues to sustain showering.
5. Pt will begin one new or resume one old leisure pursuit within physical and cognitive ability within 2 weeks.
6. Demonstrate increased compensation for R visual field issues by turning head to the right and more consistently using lighthouse techniques. Pt will report fewer incidents of running into objects on his right and knocking things over while eating.
7. Pt will begin workouts at gym 2-3x per week. Arrange for pt to meet with athletic trainer.
8. Pt will meet with vocational rehab counselor regarding work potential/ticket to work, etc.
9. Consult with neuro ophthalmologist re R visual field cut/inattention and potential with regards to driving, photography, leisure, safety. Since field cut is upper right, he could likely drive once seizures are under control at least 3 months.
10. Refer to OT driving eval.
11. Report possible depression to physician. (done today by phone)
12. Assume one parenting role that involves both leisure and appropriate supervision/discipline with children. (potentially nature walk, photography or guitar with children after consultation with wife regarding rules that were established by her in his absence).
Medical and Physician Assistant
Medical H & P Outpatient
Primary Care Provider, Tubac Community Health Center, Tubac, AZ
Dr W Smith, DO
Date: August 2, 2011
HPI:
Chip Jones is a 38-year old man who was well known to me prior to his current situation. He has been discharged from Acacia Rehabilitation Institute on August 1, 2011 following a series of events beginning on 4/19/11 following blast injuries which occurred while on patrol during a work assignment. An improvised explosive device exploded near left side of vehicle. Patient sustained blast injuries to left face and ear, left shoulder, left chest, left flank, and a compound left lower extremity fracture.
After being stabilized in local Military hospital in Afghanistan and placed in a medically induced coma he was then transferred to Landstuhl Regional Medical Center in Germany on 4/21/11.
Care in Germany included: external fixation of the compound, left mid-shaft fracture; observation and monitoring for pulmonary contusion complications and resolution; dental evaluation for broken teeth, reconstructive repair of left pinna; monitoring for closed head injury; and debridement and wound care for superficial lacerations, contusions, and abrasions. Brain MRI revealed left frontal-temporal-occipital punctate hemorrhages.
While in Germany, the patient developed pneumonia which resolved; was placed on Vancomycin and rifampin for osteomyelitis; and was placed on Dilantin for a seizure disorder.
Patient was then transferred to Gila Hospital, Tucson, AZ on 6-25-11. Vancomycin, dilantin, and pain medications were continued. An interim, removal partial dental appliance was constructed. Contractures developed in the upper and lower extremities and there was persistent edema of the right hand. He developed dizziness and continued to have tinnitus and intermittent low, grade headaches. A right sided visual defect was noted.
On July 1, 2011 Mr. Jones was transferred to Acacia Rehabilitation Institute for continued rehabilitation. During that time he fell and his cognitive issues became more apparent. He was discharged on August 1, 2011 and is to receive home health care through Cactus Home Health.
Past surgeries as a result of this set of injuries include: external fixation of an open femoral fracture, left pinna reconstruction, multiple dental extractions, debridement and wound care.
Past medical history as a result of this set of injuries include: seizure disorder, ongoing cognitive deficits, hearing loss, pain and restriction of multiple joints of the upper and lower extremities (left greater than right), osteomyelitis (healed), dental problems, depression
Allergies: NKDA
Medications: Percocet / Dilantin / Effexor / Ibuprofen
PE:
General: well nourished man who is conversant; alert and oriented to person, place, and time. Mild discomfort particularly on movement is noted.
HEENT:
Head: healed left temporal trauma.
Eyes: PERRLA, EOMI, white conjuctiva with no drainage.
Ears: ruptured left tympanic membrane with no drainage or erythema from the auditory canals. Well healed left pinna repair. Right tympanic membrane with no noted change.
Nose: no erythema or drainage. Septum midline.
Throat: gingival hyperplasia, poor dentition, mildly erythematous posterior pharynx without injection. Mildly diffuse, non-tender anterior cervical adenopathy. Trachea midline. Thyroid-moveable, nontender and without palpable masses. Carotid-no buits appreciated.
Chest:
Heart: RRR, no S3, S4, or murmurs. Lungs bilaterally clear to auscultation.
Abdomen: BS present in all four quadrants. Soft, non-tender, without masses or rebound. Rectal examination is deferred. Genital examination is deferred.
Extremities: coordinate with PT/OT
Impression:
1. Seizure disorder
2. Depression
3. s/p external fixation for an open, infected left femoral fracture with osteomyelitis-currently undergoing rehabilitation
4. S/p multiple lacerations and abrasions-healed
5. S/p left temporal fracture-healed
6. Perforated left tympanic membrane
7. Extremity contractures and restrictions
Plan:
1. Continue Dilantin, Effexor and pain medications
2. Monitor Dilantin levels and renal/liver function
3. Continue PT/OT as outpatient as needed
4. Audiology consult
5. Dental consult
6. Monitor family support and transitions
7. Osteopathic manipulative medicine
8. Follow-up once a month and/or as needed
Osteopathic
Admission Brief Osteopathic Palpatory Evaluation
Outpatient
Date: 08/02/11
Dr W Smith
Head: Occipital torsion, OM restriction left
Cervical: increased suboccipital tone, OAERrSl, C4ERrSr
Thorax: T10FRlSl
Ribcage: depressed ribs 11/12 left
Lumbar: L1ERlSl, L2FRrSr, L3FRrSr, L5ERlSl
Sacrum: lumbosacral compression
Pelvis: Left gluteal tone increased, tenderness right piriformis
Lower Extremity: tenderness right greater trochanter, restricted left hip flexion, tenderness quadriceps, hamstring tightness, posteriorly rotated left innominate
Upper Extremity: minimal edema right hand; right interosseous restriction, posterior right radial head; tender points multiple dorsal carpal.
Impression:
1. Multiple somatic dysfunctions of the head, cervical, thorax, lumbar, sacrum, pelvis, ribcage, upper and lower extremity.
2. Gait disturbance
3. Hearing loss
4 .Poor dentition
5. Seizure disorder
6. Depression
Plan:
1. OMT –Follow-up I week
2. Care per medical and surgical team
Physical Therapy
Physical Therapy
Gila Hospital – Outpatient Rehabilitation – Tucson, AZ
Initial evaluation: 9/15/11
S: Arrives to out-patient department, walking with single-point cane, accompanied by wife. “It is so good to have the fixator off of my leg. I can get around much easier now. I hope to be walking without a cane soon and want to get back to working out at the YMCA near my home.”
O: History: Multiple injuries from an IED in Afghanistan 4/19/11. Acute care in German hospital 4/21/11-6/24/11; transferred to USA and treated in Gila Hospital 6/25/11-7/1/11; In-patient acute rehabilitation at Acacia Rehabilitation Institute 7/1/11-8/1/11; Home health physical therapy 8/2/11-9/9/11. History includes closed head injury (CHI); left (L) temporal fracture; L frontal-temporal-occipital lobe punctate hemorrhages; L tympanic membrane (TM) rupture; multiple contusions and lacerations/abrasions of L scalp, face, ear, flank, leg, shoulder, chest and abdomen; contaminated, open L mid-shaft comminuted femur fracture; broken teeth; pulmonary contusion. Glasgow Coma Score of 10 initially and patient in medically-induced coma for transport to Germany. Intubated and on ventilator initially, and extubated 4/30/11. External fixator applied to L femur fracture 4/24/11; fracture remained open for healing; wound now closed and external fixator removed 9/1/11. Pneumonia 4/11 (resolved); MRSA (resolved) and osteomyelitis (Vancomycin discontinued) L LE; seizures 5/15/11 (on Dilantin); c/o tinnitus. Diagnosis of depression since injury.
Social: Married, 3 children, worked as a photo journalist. Has sunken living room, bedroom is on the 2nd floor of home (12 stairs to 2nd floor), handrail on stairs. Five steps into home and 2 handrails on stairs.
Precautions: History of seizures; FWB L LE.
Examination findings:
Cognition/language: Occasional word finding problems; high-level organization and planning problems.
Sensation: Light touch and kinesthesia intact LEs.
Motor:
PROM intact R LE, L UE, R UE; L LE: Hip flexion 5-110 degrees, knee flexion 5-80 degrees, ankle dorsiflexion 0 degrees.
Tone: Mild increased tone R plantarflexors, otherwise normal.
Strength: R UE 4+/5, R LE 5/5, L UE 5/5; L LE: 4+/5 hip flexion, 4/5 knee extension, 5/5 ankle dorsiflexion/plantarflexion. Pain 2/10 rating on PROM/AROM L knee.
Balance: Independent sitting. Maintains and reaches short distance from midline in standing without assistive device with modified independence. Occasional mild imbalance when walking on unlevel surfaces with cane.
Gait deviations: Decreased weight bearing L LE; Decreased L knee extension in stance; decreased step-length R LE; decreased heel strike L LE.
Mobility: Independent bed mobility. Standing pivot transfers to bed, chair, commode with single-point cane with modified independence. Independent wheelchair propulsion all surfaces; only uses wheelchair for long-distance ambulation. Ambulation with single-point cane 1000’ level surfaces with modified independence. Outdoor ambulation 1500’ with supervision. Supervision up and down 12 steps with single-point cane and 1 handrail with supervision.
A: Major impairments and activity limitations include:
1) Mild weakness R UE.
2) L LE limited PROM, strength and pain due to femur fracture
3) Impaired balance in walking
4) Modified independence standing pivot transfers to bed, chair, commode with cane.
5) Modified independence for ambulation on level surfaces with single-point cane.
6) Supervision for outdoor ambulation with single-point cane.
7) Supervision for stairclimbing with single-point cane and handrail.
Goals:
1) Increase strength R UE 5/5 for increased use in ADLs.
2) Increase PROM R knee flexion to 100 degrees flexion, R hip and knee extension to neutral (0 degrees); R ankle dorsiflexion to 5 degrees.
3) Independent transfers to bed, chair, commode, car without assistive device.
4) Independent ambulation indoors and outdoors all surfaces without assistive device.
5) Ascend and descend 12 steps independently.
6) Patient educated in long-term fitness program.
Plan: Therapeutic exercise and mobility training 3x/week for 4 weeks. Work with patient on plans for involvement in long-term fitness program.
Dental
Outpatient
Comprehensive Dental Examination
Patient history:
- 38 y/old male with multiple injuries from an IED in Afghanistan on April of 2011.
- Acute care in Germany hospital
- transferred to USA and treated in Gila Hospital
- In-patient acute rehabilitation at Acacia Rehabilitation
- Home health therapy
History includes head injury; L temporal fracture; L frontal-temporal-occipital lobe punctate hemorrhages; L tympanic membrane (TM) rupture; multiple contusions and lacerations/abrasions of L scalp, face, ear, flank, leg, shoulder, chest and abdomen; contaminated, open L mid-shaft femur fracture; broken teeth; pulmonary contusion. 4/2011 patient had Pneumonia (resolved); MRSA (resolved) and osteomyelitis (Gentamycin discontinued); seizures 5/15/11 (on Dilantin); Diagnosis of depression since injury.
Chief Complain:
“I want to get my teeth fixed”. Pt also requests pain medication (Percocet) after every dental treatment.
Medical history:
Seizure disorder, ongoing cognitive deficits, hearing loss, pain and restriction of multiple joints of the upper and lower extremities (left greater than right), osteomyelitis (healed), depression. Patient takes Dilantin and some pain medication.
Vitals- BP: 129/92 HR: 71
Dental history:
Patient had some extractions and lost teeth and an interim, removal partial was constructed. Broken tooth due to fall.
Extra-oral, Intra-oral, and Radiograph Examination:
OCS: Negative
EO: WNL
IO: WNL
TMJ: WNL
Hard tissue examination:
1-missing
2-existing restoration (amalgam-OL); decay on OL
3-existing restoration (amalgam-MOL); watch
4-existing restoration (amalgam-DO); -occlusal decay
5-facial fracture extending to root; decay noted; neg pulp test, neg percussion, neg palpation, neg mobility; radiolucency noted along crown suggestive of decay
6-WNL
7-missing
8-decay on distal middle 1/3
9-missing
10-incisal edge wear; notch noted sub gingival (covered by the gingiva on the Mesial)
11-cavitation on facial (cervical 1/3); neg pulp test
12-existing restoration (amalgam - DO); decay on DO
13-missing
14-existing restoration (amalgam-MO)
15-missing
16-missing
17-missing
18-missing
19-missing
20-existing restoration (amalgam - DO); recurrent decay along DO noted
21-WNL
22-WNL
23-incisal edge wear
24-incisal edge wear
25-incisal edge wear
26-WNL
27-class V decay noted
28-class V decay (wraps around distal margin)
29-missing
30-missing
31-missing
32-missing
Periodontal examination
The marginal gingiva presented rolled borders and blunted papilla.
Plaque index was 17%.
Probing depths ranged from 2-5 mm with 4-5 mm on ML/DF2, ML/MF3, DL6, DF12, MF/DF14, DL/DF20, 21, 28 along with bleeding.
Gingiva hyperplasia
Occlusal Examination:
Bilateral Angle CL 1 canine/molar relationship. 2-3 mm over jet, 1-2 mm over-bite
Etiologies:
Dry mouth, anti-seizure medication, and lack of routine dental care.
Oral risk assessment:
Caries: High
Period: moderate
Cancer: Low
